California
Californians, gay and bisexual men overrepresented in rising STD rates
‘We are sliding backward,’ says the CDC


(Photo via Bigstock)
As recently as ten years ago, the number of reported cases of chlamydia, gonorrhea, and syphilis had fallen to historic lows. In the past four years, however, data show “steep and sustained increases” in rates for all three diseases, according to the Centers for Disease Control and Prevention (CDC).
Nearly 2.3 million patients were diagnosed with chlamydia, gonorrhea, and syphilis just last year in the United States, marking the highest incidence rates of these STDs since a record-breaking number of cases were reported in 2016. Health experts warn that America is now contending with a public health crisis.
“We are sliding backward,” said Jonathan Mermin, M.D., M.P.H, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention in an Aug. 28 press release on preliminary 2017 data presented at the National STD Prevention Conference in Washington, DC. “It is evident the systems that identify, treat, and ultimately prevent STDs are strained to near-breaking point.”
STDs are treatable with antibiotics but the emergence of new drug-resistant strains of gonorrhea has challenged lines of defense that have traditionally and reliably curbed the rate of new infections. The number of new gonorrhea cases in men nearly doubled from 2016 to 2017, disproportionately among men who have sex with men (MSM).
“We expect gonorrhea will eventually wear down our last highly effective antibiotic, and additional treatment options are urgently needed,” said Gail Bolan, M.D., director of CDC’s Division of STD Prevention.
What happened? Across the board, rising rates of all three STDs can be attributed to factors that include the corresponding increase in unprotected sex among MSM, eroding public health infrastructures, clinic closures, and—to a limited extent in some groups—improved rates of STD screening.
National Coalition of STD Directors (NCSD) Executive Director David Harvey said state and local STD clinic budgets have been halved since the early 2000s. “It is time that President Trump and Secretary (Azar) declare STDs in America a public health crisis,” he said. “What goes along with that is emergency access to public health funding to make a dent in these STD rates and to bring these rates down and to ensure that all Americans get access to the health care that they need.”
While their access to sexual health resources has dwindled, research has also found gay and bisexual men are engaging in riskier behaviors, including condom-less “bareback” sex—which helps explain the rising incidence rates of chlamydia, gonorrhea, and syphilis. Experts say several factors are at play. Progress in the treatment of HIV, which is no longer considered a death sentence, may have effectively made unprotected sex “less scary.” And the introduction of pre-exposure prophylaxis (PrEP)—approved in 2012 as a once-daily regimen to reduce by as much as 99 percent the risk of contracting HIV—may have had the same effect.
Importantly, PrEP remains a valuable tool that can help reduce the number of new HIV infections, despite possible associations between use of the drug and increased risk behaviors/rates of STDs. While HIV diagnoses in the US have dropped consistently since 2010, 39,782 new cases were reported in 2016, and one of every seven patients is unaware they are HIV positive. Public health officials consider PReP a crucial resource in fighting HIV disease, and expanded access to the drug remains a core focus area in National HIV/AIDS Strategy.
To fight the STD crisis, officials have called for an approach that includes input from local stakeholders. “We don’t want to take a one-size-fits-all approach to STD prevention,” said Michael Fraser, Ph.D., executive director of the Association of State and Territorial Health Officials (ASTHO). “The techniques you might use in the MSM community are really different from what you might use with pregnant women…And I think that’s another place where states have a lot of expertise because they know their population and they know some of the stuff that works well in some of those areas.”
State-specific data will be made available after the CDC publishes the full surveillance report in September. But public health workers in California have already reported spikes this year in the number of diagnosed cases of STDs, particularly of syphilis among gay and bisexual men.
Overall, according to CDC data from 2016, California has the third-highest number of reported syphilis cases in the country. Compared with the national rate, about 8.7 cases per 100,000 people, California—at 15 cases per 100,000—is more than 72 percent higher. And in San Francisco County, 60.4 cases were diagnosed for every 100,000 people, which exceeds by nearly seven times the national rate.
In May 2018, the Riverside County Department of Public Health also reported the number of cases in the Coachella Valley had risen dramatically—mostly in populations of MSM. And Palm Springs exceeded by more than 10 times the national incidence rate.
The Riverside University Health System has started hosting community meetings with key stakeholders to address the county’s syphilis outbreak. Program Coordinator Tad Berman told the Los Angeles Blade the third and fourth meetings are scheduled for Sept. 10 and 11. “The general public is welcome to come and provide input,” he said. “It’s important to get their feedback to make sure that, in our messaging, that we are speaking the language of the public.”
| Spotlight on Syphilis
Monday Sept. 10, 2018, 1:30 p.m. UCR Palm Desert Building B 75080 Frank Sinatra Drive Palm Desert, CA 992211 |
Spotlight on Syphilis
Tuesday Sept. 11, 2018, 1:30 p.m. Community Action Partners (CAP) 2038 Iowa Avenue, B 101 Riverside, CA 92507 |
Los Angeles County
New on the LA County Channel
You can watch on Channel 92 or 94 on most cable systems, or anytime here. Catch up on LA County Close-Up here
New on the County Channel

L.A. County is investing millions of dollars in American Rescue Plan funds for paid early education apprenticeships. The Early Care and Education Assistant Teacher Apprenticeship Program aims to bolster the education career pipeline and bring relief to those hoping to avoid financial debt.
You can watch more stories like this on Channel 92 or 94 on most cable systems, or anytime here. Catch up on LA County Close-Up here.
In Case You Missed It
April is “Sexual Assault Awareness Month”
This April marks the 23rd observance of Sexual Assault Awareness Month. Sexual Assault Awareness Month is a chance for each of us to think about the role we can play in preventing sexual abuse, assault, and harassment.
Violence is preventable. Stopping sexual abuse, assault, and harassment before they happen requires us to work together to support healthy, safe, and respectful behaviors and environments. To build truly connected communities, we must start with community accessible services and support and expand the network of service providers. When it comes to sexual violence, everyone has a role to play to help build a community that is safer, inclusive, and equitable. Below are some resources and ways for you to get involved:
- Raise Awareness: The National Sexual Violence Resource Center
- Participate in Denim Day | April 24, 2024: 5 Ways to Participate in Denim Day and Denim Day Rally & Press Conference
- Learn More: Office of Family Violence Prevention and Services and The Rape, Abuse, and Incest Network (24/7 Confidential Support Hotline)
If you or someone you know has been sexually assaulted, call the National Sexual Assault Hotline: 1-800-656-4673.
Learn more at lacounty.gov/sexual-assault-awareness-month/.
At Your Service
Commercial Acquisition Fund Program

The Los Angeles County Department of Economic Opportunity recently launched the Commercial Acquisition Fund to provide grants to qualifying nonprofit organizations to support the acquisition of vacant or abandoned land and buildings in designated communities that were most negatively impacted by the COVID-19 pandemic.
The Commercial Acquisition Fundis funded by the County, with $10 million in American Rescue Plan Act funds and will be awarded as recoverable grants, ranging from $500,000 to $2,000,000. Acquisitions and funding must occur before December 1, 2024.
To learn more, apply, or sign-up to attend a community webinar, visit lacaf.info.
Out and About
April 21 – April 27th is “National Crime Victims’ Rights Week”
Join District Attorney George Gascón, the LA District Attorney’s Bureau of Victim Services and the LA District Attorney Crime Victims Advisory Board for this special National Crime Victims’ Rights Week panel discussion: “Pathways to Healing: Supporting LA’s Crime Survivors.”
This hybrid event will be on Thursday, April 25 at 6 PM, with doors opening at 5:30 PM. Click here to register to attend.
Photo Finish

Celebrate the 4th year of SOAR at the South Coast Botanic Garden when butterflies return May 1!
Click here to access more photos of LA County in action.
West Hollywood
City of West Hollywood is hosting a Public Safety Open House
The open house is an opportunity to engage as a community to prioritize safety and well-being along with WeHo Public Safety partners
By Paulo Murillo | The City of West Hollywood is partnering with the West Hollywood Sheriff’s Station, Block By Block Security, Los Angeles County Fire Department and Public Safety Commissioners for a Public Safety Open House on May 1, 2014, beginning at 6:00 p.m. at Plummer Park, Room 5 at 7377 Santa Monica Boulevard. The open house is an opportunity to engage as a community to prioritize safety and well-being along with our Public Safety partners.
The event is being billed as an informal meeting to interact with Public Safety partners and Commissioners, learn about available resources, and discover ways to actively contribute to keeping West Hollywood a safe place for everyone. The event will also be serving pizza, salad, and refreshments, with vegan options available.
The Public Safety Commission was created on September 18, 1989 and is comprised of five (5) members, appointed by individual Councilmembers, and two (2) members appointed by the Council as a whole (at-large). Each member of the Commission shall serve a two-year term commencing March 1st following a general municipal election. Members shall be residents of the City and shall not be officers or employees of the City. The Commission shall meet no more than once monthly, and if a member of the Commission is absent for any reason for more than three regular meetings in any twelve-month period, the office of such member shall be vacated.
The Public Safety Commission shall evaluate and recommend mechanisms involving public safety issues, assist the City Manager’s office and City Council in strengthening community response to emergencies, evaluate and make recommendations to City Council regarding neighborhood livability and domestic violence prevention.
The West Hollywood Sheriff’s Station is part of the Los Angeles County Sheriff’s Department and provides essential law enforcement services for the community. If you need to file a crime report online, you can do so through the SORTS system. Captain William Moulder leads the station, ensuring safety and security for residents and visitors alike.
The Los Angeles County Fire Department (LACoFD) provides firefighting and emergency medical services for the unincorporated parts of Los Angeles County, California, as well as 59 cities through contracting, including the city of La Habra, which is located in Orange County and is the first city outside of Los Angeles County to contract with LACoFD
Block by Block Security Ambassadors is a program in the City of West Hollywood that provides a highly visible uniformed presence at the street level. The program was first established in 2013. The ambassadors are deployed on bicycles or on foot along major streets, alleys, City parking lots, and residential neighborhoods. They work in collaboration with the West Hollywood Sheriff’s Station to provide supplemental safety services. The ambassadors provide safety escorts, conduct foot and bicycle patrols, and offer helpful guidance to community members and visitors.
******************************************************************************************

Paulo Murillo is Editor in Chief and Publisher of WEHO TIMES. He brings over 20 years of experience as a columnist, reporter, and photo journalist. Murillo began his professional writing career as the author of “Love Ya, Mean It,” an irreverent and sometimes controversial West Hollywood lifestyle column for FAB! newspaper. His work has appeared in numerous print and online publications, which include the “Hot Topic” column in Frontiers magazine, where he covered breaking news and local events in West Hollywood. He can be reached at [email protected]
The preceding article was previously published at WeHo Times and is republished with permission.
Southern California
Triple A: Gas price increases slow down
The average price for self-serve regular gasoline in California is $5.45, which is four cents higher than a week ago

LOS ANGELES – Southern California gas prices are still up for the week, but are not increasing as quickly as they were earlier this month, according to the Auto Club’s Weekend Gas Watch. The average price for self-serve regular gasoline in California is $5.45, which is four cents higher than a week ago. The average national price is $3.67, which is also four cents higher than a week ago.
The average price of self-serve regular gasoline in the Los Angeles-Long Beach area is $5.39 per gallon, which is three cents more than last week, 43 cents higher than last month, and 44 cents higher than last year. In San Diego, the average price is $5.38, which is four cents higher than last week, 44 cents higher than last month, and 44 cents higher than this time last year.
On the Central Coast, the average price is $5.35, which is four cents higher than last week, 41 cents higher than last month, and 43 cents higher than last year. In Riverside, the average per-gallon price is $5.32, which is five cents higher than last week, 49 cents higher than last month and 46 cents higher than a year ago. In Bakersfield, the $5.31 average price is seven cents more than last week, 48 cents more than last month, and 42 cents higher than a year ago today.
“According to Oil Price Information Service (OPIS), yesterday’s U.S. Energy Information Administration report showed that West Coast gasoline inventories are at their lowest level in two years,” said Auto Club Spokesperson Doug Shupe. “However, OPIS also reported that imported gasoline should be on its way to California in the next few weeks, which should help ease the upward pressure on pump prices.”
The Weekend Gas Watch monitors the average price of gasoline. As of 9 a.m. on April 18, averages are:

Los Angeles County
UCLA survey says quality of life in L.A. County is way down
High cost of housing is the most important factor impacting the annual Quality of Life Index, particularly among renters

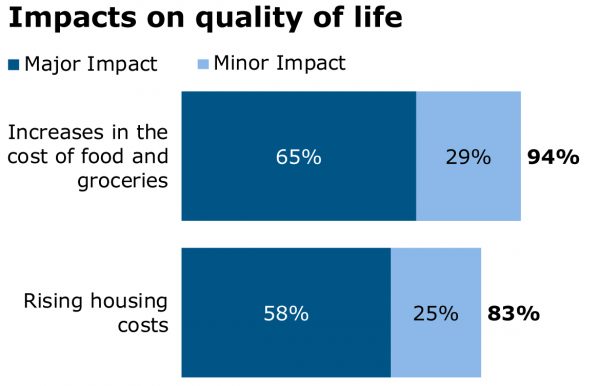
LOS ANGELES – Affordable housing, groceries and consumer goods that have all spiraled upward in cost has lowered the quality of life for Los Angeles County residents this past year according to a survey conducted by UCLA’s Luskin School of Public Affairs.
Interviews were conducted with 1,686 L.A. County residents between Feb. 22 and March 14, both in English and Spanish.
The Quality of Life Index, or QLI, is a project of the Los Angeles Initiative at the UCLA Luskin School of Public Affairs measures county residents’ satisfaction in nine categories. The overall rating fell two points from last year to 53 on a scale from 10 to 100, marking the second time in three years it came in below the survey’s 55 midpoint since the index launched in 2016. That means a majority of respondents are dissatisfied with the overall quality of their lives.
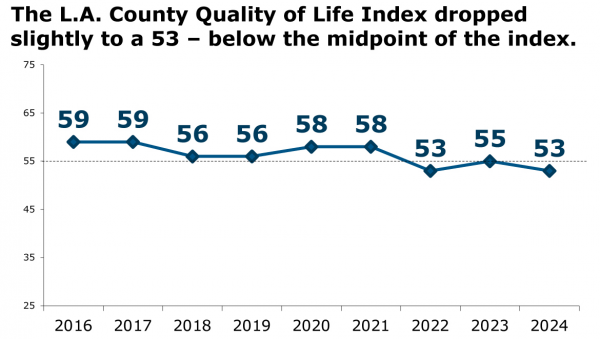
Zev Yaroslavsky, director of the study at UCLA said renters, who make up nearly half of survey respondents, are being disproportionately affected by the economic and inflationary pressures facing the region. More than half, or 59%, cited housing as the most important factor in their rating.
“Housing costs have gone up,” Yaroslavsky said. “And incomes have not gone up anywhere near commensurate with what’s happened to housing.”
While 61% of homeowners feel optimistic about their economic future in Los Angeles County, 51% of renters report being pessimistic. Only 23% of renters think they will be able to buy a home where they would want to live at some point in the future.
KTLA reported that according to data released by the National Association of Realtors earlier this year, parts of L.A. County rank 8th highest in the nation for highest housing prices. Just 23% of the renters that responded to the survey believed that they’d be able to buy a home in an area they find desirable in the future.
Homelessness problems are worsening
This year’s survey also produced striking results on the issue of homelessness.
“We discovered very little optimism about whether the current programs and efforts to eradicate homelessness will work,” Yaroslavsky said.
More than half, or 60%, of respondents said homelessness in their area has gotten worse over the past year, with only 10% saying it has gotten better. Just 20% are more hopeful than they were last year that the homelessness situation in Los Angeles County will improve.
Respondents were also asked whether they worried about becoming homeless themselves, with the highest levels of anxiety expressed by people living in households earning less than $60,000 annually at 44%, renters 37% and African Americans 33%.
“Despite the best efforts of state and local officials, the public is more negative and less hopeful about solving homelessness,” Yaroslavsky said.
In an email to the Blade Wednesday, Chair of the Los Angeles County Board of Supervisors Lindsey Horvath said:
“Watching my neighbors struggle with affordability or be on the brink of homelessness is what calls me to be of service to our community. We need to urgently address our overlapping homelessness and affordable housing crises by expediting production of all forms of housing, expanding tenant protections, and ensuring fair wages to address rising income inequality.”
Dissatisfaction with the government
Noting the fact that this is an election year Yaroslavsky, a former member of the Los Angeles County Board of Supervisors from December 1, 1994 – December 1, 2014, said: “It feeds an overall sense that things aren’t working well.”
He framed this year’s results in the context of nearly a decade’s worth of research showing positive results for neighborhood quality and racial/ethnic relations, but low marks in categories commonly associated with decisions by public officials.
“A main theme over the last nine years is that Angelenos love the neighborhoods where they live. We appreciate diversity and get along with others better than some people think. And the quality of life for most of us is pretty good,” he said. “But at some fundamental level, people think our governmental institutions are letting them down.”
The last year has seen a modest decline in most ratings for elected officials.
- Los Angeles County Sheriff Robert Luna is viewed favorably by 34% and unfavorably by 26%. Last year was 37% favorable and 21% unfavorable.
- Los Angeles Mayor Karen Bass is viewed favorably by 42% and unfavorably by 32%, a drop from 46% favorable and 23% unfavorable in last year’s QLI.
- Respondents had a slightly favorable view of the city councils in their cities: 37% favorable and 32% unfavorable. The Los Angeles County Board of Supervisors is viewed more negatively: 27% favorable and 35% unfavorable.
The Quality of Life Index in issues regarding the environment found that 25% of respondents said climate change had a major impact on their quality of life in the last year; 38% saw a minor impact.
West Hollywood
Family demanding answers in beating of gay hair stylist in WeHo
The family questions why it taking so long for West Hollywood Sheriff’s station to retrieve video footage from local businesses

By Paulo Murillo | LOS ANGELES – Friends, family, and supporters of 54-year-old Albert Vasquez, a celebrity hairdresser found brutally beaten in West Hollywood’s Rainbow District on April 5, 2024, continue to demand answers and call for justice as they try to piece together what happened on that fateful Friday night.
Vasquez was discovered unconscious on the ground with severe head trauma, a black eye, and scrapes and scratches to his arms and legs in a parking lot behind Heart WeHo at 8911 Santa Monica Blvd, in West Hollywood’s Rainbow District.
The family questions why it taking so long for West Hollywood Sheriff’s station to retrieve video footage from local businesses. They also don’t understand why the Sheriff’s Station suggested to media outlets that Albert could have possibly fallen and gotten injured without investigating or knowing any details about his injuries.
Questions have also arisen regarding Heart WeHo, the last nightclub where Albert was allegedly seen on the night of the attack, reportedly after leaving Gym Bar according to witnesses. In efforts to solve the mystery surrounding the attack, supporters have taken to social media to demand that Heart WeHo, partly owned by celebrity entrepreneur Lance Bass of the boyband NSYNC, deliver unedited footage to detectives at the West Hollywood Sheriff’s Station.
The calls for video footage and threats to have a protest outside of Heart WeHo prompted Heart to issue a statement.
“Heart WeHo remains deeply committed to the safety and wellbeing of our community. We are aware of the incident that occurred on April 5th and have been actively collaborating with the West Hollywood Sheriff’s Department to assist in their investigation since the beginning. We have provided the authorities with unrestricted access to our security footage,” reads the statement by Heart WeHo. “We urge anyone with additional information pertaining to this incident to come forward and assist the West Hollywood Department in their efforts to ensure the safety and security of our neighborhood.”
The victim’s sister, Gloria Jimenez, tells WEHO TIMES that Heart WeHo turned over surveillance footage to the West Hollywood Sheriff’s Station on Monday, ten days after the incident occurred.
“I was hoping people would speak up or that somebody has video or something,” she said. “Everybody’s always videotaping, and we haven’t gotten anything at all. We’re really just relying on the police to expose that footage but there are all these rules and regulations where you cannot get it yourself. You have to wait for police to collect it and we were after the police to do something and they just got the footage yesterday [Monday].”
Regarding updates on Albert’s injuries, Ms. Jimenez says that doctors discovered a second skull fracture on the other side of his head. He also has bruised lungs, which went unnoticed throughout his stay at the hospital. These injuries are in addition to a black eye and scratches on his legs and arms, and it appears he was kicked in the neck.
However, despite his newly discovered injuries, Albert seems to be on the mend, she said. He was in a coma for one day when he was brought to the hospital, but is currently awake and seems to be aware of his surroundings. He starts therapy this week and is expected to be in the hospital for another week and a half. He has not spoken about what happened to him that Friday night, mainly because he’s heavily medicated and nurses feel it’s too soon to pressure him to relive the trauma.
Jimenez’s story has garnered national and global attention. His attack was published in the Daily Mail, and there is a campaign of supporters asking for justice for Albert, who is widely known in the West Hollywood community.
Ms. Jimenez alleges that they have received several tips alleging Albert was last seen at Gym Bar when he was there with friends and then he headed to Heart WeHo, which is the last time they saw him. She said in addition to the footage at Heart WeHo, she is also going to seek footage from Gym Bar to determine what time he left and in which direction he headed.
There were also some witnesses stating that he was heavily intoxicated and that he had a confrontation with one of the securities at Heart WeHo, but that has not been confirmed. The surveillance video will answer that question.
Ms. Jimenez thanks the community for their support and for being relentless in holding investigators accountable and demanding they get answers. She’s also grateful for the public’s generosity to help cover medical expenses.
Anyone with information is asked to reach out to West Hollywood Detective Franklin at (310) 855-8850.
The family’s GoFundMe campaign: (Link)
******************************************************************************************

Paulo Murillo is Editor in Chief and Publisher of WEHO TIMES. He brings over 20 years of experience as a columnist, reporter, and photo journalist.
******************************
The preceding article was previously published by WeHo Times and is republished with permission.
Los Angeles County
Eric Schockman appointed to LA County LGBTQ+ Commission
Schockman served as high-level staffer in the State Assembly & was instrumental in passing AB 1 (1st LGBTQ+ civil rights bill in California)
LOS ANGELES – Los Angeles County Assessor Jeff Prang appointed LGBTQ+ community leader and educator as well as noted author H. Eric Schockman, Ph.D., to the first-ever Los Angeles County LGBTQ+ Commission.
Schockman currently is Professor of Politics and International Relations at Woodbury University, previously serving as Associate Dean and Associate Adjunct Professor at the Sol Price School of Public Policy at the University of Southern California.
He was President and founder of the Global Hunger Foundation, dedicated to helping women in the developing world break the chains of poverty by funding projects designed to provide sustainable development and organic farming. He served as CEO and President of a prestigious international anti-hunger organization for over a decade pumping some $60 million in grants into the field.
“This was an easy choice for this ground-breaking commission,” Los Angeles County Assessor Prang said. “I’m just grateful that Eric agreed to serve on this important commission, especially in light of the serious and hateful policies against the LGBTQ+ community across the country. Eric has a long record of leadership and activism, advocating for LGBTQ+ equality and will add a strong voice of experience and accomplishment to this important commission.”
Schockman served as high-level staffer in the State Assembly and was instrumental in passing AB 1 (the first LGBTQ+ civil rights bill in California). He has also written several books and edited many articles on leadership and politics in California, the nation and international affairs, and presented on scholarly panels on these same topics.

(Photo Credit: Woodbury University)
Schockman holds a Ph.D. in Political Science and International Relations from the University of California.
“I am pleased and honored to be asked to serve on this historic commission,” Schockman said. “Assessor Prang has shown his leadership in LGBTQ+ issues for years and I do not take this new assignment lightly. I am grateful to be selected.”
The Commission was created last June with a motion authored by Supervisors Hilda L. Solis and Janice Hahn. The 15-member Commission will provide recommendations on policies and budget priorities at a time when LGBTQ+ people face mounting challenges.
According to the LA County Commission on Human Relations’ 2021 Hate Crime Report, 89% of the hate crimes towards gay men were of a violent nature and 93% of anti-transgender crimes were violent – a rate of violence higher than any other marginalized group recorded by the report.
The Los Angeles County LGBTQ+ Commission will be seated and hold its first meeting in the coming months.
West Hollywood
WeHo City Council Votes to affirm minimum wage of $19.08
The minimum wage increase is determined by the Consumer Price Index for for the Los Angeles-Long Beach-Anaheim, areas

By Paulo Murillo | WEST HOLLYWOOD – At a Regular West Hollywood City Council meeting on Monday, April 15, 2024, the City Council voted to affirm the City’s Minimum Wage rate of $19.08 per hour and current Leave Provisions through December 31, 2024.
Council member John Heilman made a motion to ask City Staff to come back with an ordinance change that will make the Consumer Price Index (CPI) increase annual starting in January. the motion was seconded by council member Lauren Meister. The motion passed 4-1 with a no vote from council member Sepi Shyne.
The City of West Hollywood breaks down the City’s minimum wage ordinance as follows:
How is the CPI increase determined?
The minimum wage increase is determined by the Consumer Price Index for Urban Wage Earners and Clerical Workers (CPI-W) for the Los Angeles-Long Beach-Anaheim, CA area.
According to the Resolution establishing an annual minimum wage increase, the minimum wage increase shall be no less than 1.0% and no more than 4.0%.
Compensated and Uncompensated Leave
Full time employees for all businesses are to be provided at least 96 compensated hours and 80 uncompensated hours per year for sick leave, vacation, or personal necessity. Part-time employees are to be provided compensated and uncompensated hours in increments proportional to that accrued by someone who works 40 hours in a week.
Administrative Regulations
To provide West Hollywood Employees and Employers further clarification on implementing the Minimum Wage Ordinance, the City has published Administrative Regulations. The Administrative Regulations outline guidance related to payment of the Citywide Minimum Wage, Compensated and Uncompensated Leave, and application of a waiver for certain Employers.
Legal Notices
Every Employer in the City of West Hollywood shall post in a conspicuous place at any workplace or job site where any Employee works, the bulletin published each year by the City informing Employees of the current minimum wage rate and of their rights under the Ordinance. Every Employer shall post notices in English, Spanish, and any other language spoken by at least five percent (5%) of the Employees. Every Employer shall also provide to each Employee at the time of hire, the Employer’s name, address, and telephone number in writing.
July 1, 2023 Minimum Wage Notices
- All Business Minimum Wage Poster (English / Spanish / Russian)
- Hotels Minimum Wage Poster (English / Spanish / Russian)
Waiver Application
A one-year waiver may be granted to businesses who are able to demonstrate that compliance with the payment of the Citywide Minimum Wage would force the business to: file bankruptcy or a shutdown, reduce its workforce by more than twenty percent (20%), or curtail its Employees’ total hours by more than thirty percent.
A one-year, one-time waiver may be granted to businesses who are able to demonstrate that compliance with the leave provisions of the Citywide Minimum Wage would force the business to: file bankruptcy or a shutdown, reduce its workforce by more than twenty percent (20%), or curtail its Employees’ total hours by more than thirty percent.
Alternatively, a three-month waiver may be granted to businesses who are able to demonstrate that compliance with the leave provisions of the Citywide Minimum Wage would cause an implementation hardship due to my business’ existing payroll and human resources processes and platforms the business has in place. Businesses may apply for up to two three-month waiver (maximum of six months)
To file your waiver application, please follow these steps:
- Notify all your employees, in writing, of the business’ intent to file a Waiver Application
- Compile all required documents – incomplete applications will be denied
- Submit the Waiver Application and all required documents by selecting the waiver for payment of minimum wage or leave provisions:
******************************************************************************************

Paulo Murillo is Editor in Chief and Publisher of WEHO TIMES. He brings over 20 years of experience as a columnist, reporter, and photo journalist.
******************************
The preceding article was previously published by WeHo Times and is republished with permission.
Southern California
USC cancels valedictorian’s speech over antisemitism allegations
“I am shocked by this decision & profoundly disappointed that the university is succumbing to a campaign of hate meant to silence my voice”

LOS ANGELES – The University of Southern California (USC) has decided to cancel the commencement speech of Asna Tabassum, a pro-Palestinian undergraduate and this year’s valedictorian, citing safety concerns. This decision marks the first time in the university’s 141-year history that a valedictorian has been prohibited from speaking at the graduation ceremony.
Provost Andrew Guzman expressed that while disappointing, the decision was necessary to ensure the safety of the campus and its students, emphasizing that the university’s actions are aligned with legal obligations to maintain a secure educational environment. He also clarified that the decision does not infringe upon free speech rights, as there is no entitlement to speak at the event.
Tabassum, majoring in biomedical engineering with a minor in “resistance to genocide,” faced criticism for her online posts about the Middle East conflict. The controversy escalated when a pro-Israel group accused her of antisemitism less than a week ago.
In response to the cancellation, the Council on American-Islamic Relations-Los Angeles (CAIR-LA) has called for the decision to be reversed, allowing Tabassum to deliver her speech. Tabassum, through CAIR-LA, stated that she has been subjected to a campaign of racist hatred due to her stance on human rights.
In a statement released through the Council on American-Islamic Relations-Los Angeles (CAIR-LA), Tabassum conveyed her shock and profound disappointment at the university’s decision, stating it was a result of a “campaign of hate” aimed to silence her voice. “Anti-Muslim and anti-Palestinian voices have subjected me to a campaign of racist hatred because of my uncompromising belief in human rights for all,” Tabassum said.
USC maintains that the decision was solely based on safety considerations and not on the content of Tabassum’s proposed speech or her political views. The university has consulted its public safety department and external safety experts, concluding that the potential risks necessitate the cancellation for this year’s commencement to focus on celebrating the graduates without disruptions.

Tabassum’s full statement:
“I am honored to have been selected as USC Class of 2024 Valedictorian. Although this should have been a time of celebration for my family, friends, professors, and classmates, anti-Muslim and anti-Palestinian voices have subjected me to a campaign of racist hatred because of my uncompromising belief in human rights for all.
“This campaign to prevent me from addressing my peers at commencement has evidently accomplished its goal: today, USC administrators informed me that the university will no longer allow me to speak at commencement due to supposed security concerns. I am both shocked by this decision and profoundly disappointed that the University is succumbing to a campaign of hate meant to silence my voice.
“I am not surprised by those who attempt to propagate hatred. I am surprised that my own university—my home for four years—has abandoned me,” Tabassum wrote.
Related:
Los Angeles
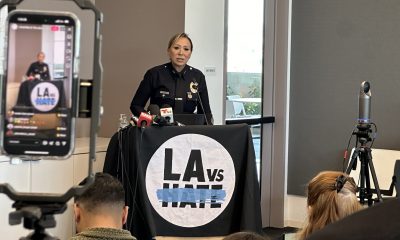
LA leaders call for unity & protection for trans community
LAPD has noted a 13 percent increase in overall hate crimes, with LGBTQ+ specific hate crimes up by 33 percent

LOS ANGELES – Addressing a concerning escalation of threats against LGBTQ+ organizations throughout the country, leaders from TransLatin@ Coalition, the Los Angeles Police Department, and other officials gathered in a press conference to denounce acts of intimidation and to call for unity and protective measures for the trans and queer community.
A bomb threat called in to the LAPD on March 28, aimed at the TransLatin@ Coalition specifying today April 15 as the target date, has prompted an immediate and ongoing response from local authorities to ensure the safety of those at the coalition’s facilities and others. The LAPD has since been closely monitoring the site.
The suspect, identified as Henry Nolkemper, a white 61 year old male, was arrested by LAPD shortly afterward after being observed entering his residence on West 53rd Street. The police then searched his residence. Despite the absence of explosives, he was booked under serious charges including criminal threats with a hate crime enhancement.
Nolkemper, known to have a history of mental health issues, was on parole for previous threats to the community. His parole has since been revoked and he is currently held on a one million dollar bail.
The press conference today began with remarks from Robin Toma, Executive Director of LA vs Hate, who highlighted the organization’s role as the third largest source of hate crime reporting in Los Angeles, trailing only police sources.
He also stated that LA vs Hate has reported a troubling increase in trans-specific crimes, noting that such incidents are grossly underreported, a sentiment echoed by surveys within the trans community.

Bamby Salcedo, President and CEO of TLC, expressed her gratitude for the continued support from various partners and emphasized the daily challenges faced by transgender individuals. “Every day a trans woman steps out of her home, it is a revolutionary act. We are people who walk with targets on our backs,” Salcedo declared, setting a tone of resilience and defiance against the threats.
Special thanks were given to Supervisor Hilda Solis and Jury Candelario, a partner from APAIT and a Filipino immigrant, who marked 35 years in America by calling the trans-related stress “chronic” in his long tenure as a social worker. Esther Lim, representing Supervisor Solis, condemned the bomb threat as an act of “cowardice” and highlighted Solis’ support through a previous $55,000 contribution to TLC and a new motion to establish LA’s first LGBTQ+ commission.
Assistant Chief Blake Chow and Deputy Chief Ruby Flores of the LAPD provided updates on the legal actions following the threat. They noted a 13 percent increase in overall hate crimes, with LGBTQ+ specific hate crimes up by 33 percent. “Behind each hate crime, there is a victim, there are families,” Flores said, urging the community to report incidents and support anti-hate education initiatives. “These crimes affect people in ways statistics can’t reflect.”
The press conference also featured voices from the community like Mariana Marroquin, Associate Director of Trans Wellness, who spoke passionately about the ingrained nature of hate experienced by trans individuals from a young age, and Cari Maddox, who emphatically stated, “Hate has no home in Los Angeles.”
Mark Bayard, representing Los Angeles County District Attorney George Gascon, affirmed the DA’s commitment to fighting hate crimes vigorously, especially in light of the upcoming election season, which often sees a spike in such incidents.
As the community grapples with this latest threat, the message from today’s conference was clear: solidarity, education, and legal protection are key to combating hate and fostering a society where transgender people can integrate fully and safely.
Riverside County
Riverside County school district kills trans outing policy
MVUSD’s forced outing policy is identical to the Chino Unified School District policy which a judge described as “discriminatory on its face”

MURRIETA, Calif. – The Murrieta Valley Unified School District Board (MVUSD), abandoned its controversial policy that would have forced school faculty and staff to “out” trans and non-binary students to parents.
In an emailed sent out Friday to parents, faculty, and staff members, school district administrators noted that the policy was reversed.
The California Department of Education found that it violated the state’s education codes and warned MVUSD that the policy “provided no educational or administrative purpose that could justify the discrimination of LGBT+ students.” The Department of Education stated the policy “singles out and is directed exclusively toward one group of students based on that group’s legally protected characteristics of identifying with or expressing a gender other than that identified at birth.”
In its email, MVUSD noted that the policy “is inconsistent with Education Code Section 220 and for this reason the mandatory notification requirements set forth in BP 5020.1 will not be implemented.”
Last month the MVUSD school board voted 3-2 to keep the forced outing policy on the books even though, according to a Press-Enterprise report, MVUSD Board President Paul Diffley was warned by the district’s law firm, Atkinson, Andelson, Loya, Ruud & Romo (AALRR), that “‘going ahead (with the policy) in such an environment’ could cost the district $500,000 in legal expenses.”
After the board vote, two district educators, Jamie Goebel and Karen Poznanski, filed a complaint with the California Department of Education about the policy due to its “discrimination on the basis of gender identity and expression.”
“This policy not only violated the privacy and dignity of our students but also perpetuated harm and discrimination against LGBTQ+ individuals and their families,” Poznanski told the Press Enterprise once the California Department of Education sided with the teachers last week.
MVUSD’s forced outing policy is identical to the policy passed by Chino Unified School District (CVUSD) that California Superior Court Judge Michael Sachs described as “discriminatory on its face” and placed under a preliminary injunction in October 2023.
The lawsuit, The People of the State of California, Ex Rel. et al -v- Chino Valley Unified School District (San Bernardino County Superior Court Case No. CIVSB2317301), was introduced by California Attorney General Rob Bonta on August 28, 2023, and was placed under a temporary restraining order on September 6, 2023 prior to the October ruling.
-

 Political commentary & analysis3 days ago
Political commentary & analysis3 days agoThe Cass Review heralds how all trans medicine will die
-

 West Hollywood4 days ago
West Hollywood4 days agoOut stylist found beaten outside Heart WeHo nightclub recovering
-

 Sports2 days ago
Sports2 days agoWNBA star Brittney Griner & wife Cherelle expecting first child
-

 West Hollywood23 hours ago
West Hollywood23 hours agoFamily demanding answers in beating of gay hair stylist in WeHo
-

 Political commentary & analysis3 days ago
Political commentary & analysis3 days agoEU elections, empowering queer women & need for safe spaces
-

 North Carolina4 days ago
North Carolina4 days ago“Rainbow Story Time” gets bomb threat, closes Durham N.C. library
-
 Los Angeles3 days ago
Los Angeles3 days agoLA leaders call for unity & protection for trans community
-

 Travel4 days ago
Travel4 days agoHot fun in the desert sun: Your Palm Springs guide
-

 Research/Study2 days ago
Research/Study2 days agoRight-wing pastor & podcast host: LGBTQ movement equals Hitler
-

 Riverside County3 days ago
Riverside County3 days agoRiverside County school district kills trans outing policy












