Commentary
Call a doctor. Call a doctor, now.
Is the CDC ready for another pandemic?


Christopher M. Kane is a freelance writer with a professional background in nonprofit communications, most recently, with organizations in the healthcare/research space. He lives with his husband in Washington, D.C. (Photo provided by Kane)
Call a doctor, preferably, one who’s employed by a government agency that was created to respond to mass casualty pandemic illness. Do it while you still can.
There was a major uproar in December when the Washington Post reported that that the Trump administration had ordered the Centers for Disease Control and Prevention (CDC) not to use “seven dirty words”—“vulnerable,” “entitlement,” “diversity,” “transgender,” “fetus,” “evidence-based” and “science-based.”
But a week later, Slate revealed the supposedly banned words were in fact selected by CDC career employees, not political appointees, in an effort to protect funding for their research.
Think about that. And think about how it’s consistent with the Trump administration’s tendency to curb the influence of experts and deny epistemic knowledge. Of far greater concern than the threat of terrorism is the inevitability of another virus that could make AIDS look like conjunctivitis.
To advance his immigration agenda, President Trump claimed all Haitians have AIDS, according to the New York Times, a remark the White House disputes, of course. But it tracks with his familiar racism and insensitivity. It also displays a shocking lack of understanding about public health and disease.
In “AIDS and its Metaphors,” Susan Sontag cautioned against “many of the enduring Eurocentric presumptions about others, starting from the fantasy that peoples with little reason to expect exemption from misfortune have a lessened capacity to feel misfortune.”
Writing before epidemiologists knew for certain where AIDS began, Sontag explained: “The fact that illness is associated with the poor…reinforces the association of illness with the foreign: with an exotic, often primitive place. Illustrating the classic script for plague, AIDS is thought to have started in the ‘dark continent,’ then spread to Haiti, then to the United States and to Europe.
Africans who detect racist stereotypes in much of the speculation about the geographical origin of AIDS are not wrong.”
A virus doesn’t discriminate against potential hosts and in an interconnected world with some 44,000 airports, the question is not whether a contagious disease will spread across oceans but rather when and how quickly. All affected communities, regardless of their relative wealth, will suffer terribly from the next pandemic.
I choose the word “next” deliberately. Americans in this moment are dealing with a flu outbreak poised to be as destructive as in the 2014-2015 season, the worst in recent years. And the Ebola virus, whose origins also trace back to the African continent, remains a potent threat.
And herein lies the concern with Trump.
In 2014, a Liberian national unwittingly brought Ebola to the United States and under the wise counsel of public health officials, the Obama administration decided against administering travel bans. They would not have effectively prevented all people infected with the disease from entering the country and only would have worsened the situation by cutting off the supply of international aid workers to affected countries that, generally, have limited resources and a limited ability to contain the outbreak.
When American health workers were dispatched to Liberia that year and returned stateside for treatment after they contracted Ebola, Trump tweeted: “Ebola patient will be brought to the U.S. in a few days – now I know for sure that our leaders are incompetent. KEEP THEM OUT OF HERE!”
The president has a clear affinity for travel bans. And there’s every reason to expect that if an outbreak develops under his administration, Trump will pursue this against the advice of doctors and researchers and healthcare workers who have already explained why it’s a terrible idea.
This would unfold amid a fraught political climate. The CDC, the agency tasked with containing pandemics, has felt such a chilling effect from the top that employees were compelled to edit out seven words with which, they assumed, the Trump administration is likely to take issue. Among these, “evidence-based” and “science-based.”
Meanwhile, the CDC has 700 vacancies, including “several positions in the Office of Public Health Preparedness and Response, which regulates some of the world’s most dangerous bacteria and viruses and manages the nation’s stockpile of emergency medical countermeasures,” according to the Washington Post.
Read Richard Preston’s “Crisis in the Hot Zone” to see how close we came to a catastrophically deadly Ebola pandemic. It chronicles how brave government workers contained an outbreak of Ebola Reston, so named for the Washington, D.C. suburb in which it was discovered. It could have been as virulent as Ebola Zaire, a nearly identical virus that killed 90 percent of patients affected in a 2003 outbreak. It could also have happened under a government that disenfranchised those researchers, scientists, and doctors who are our only hope.
Preston was told by an expert that Ebola is “interesting”—in the sense that one can call “interesting” the prospect of being confronted by a cobra that’s agitated and poised to strike.
Amid new revelations that have intensified doubts about the president’s fitness for office, it’s time to assess our nation’s preparedness for an outbreak of pandemic illness. It’s time to revisit the lessons learned from AIDS, as well as close calls with Ebola and Influenza.
It’s time to let doctors and researchers do their job of protecting us and the nation without fear of political retaliation.
Commentary
Breaking the mental health mold with Ketamine: insights from creator of Better U
How this brand is making high-impact mental health care available to the people who need it most

Ketamine therapy was once on the fringe, but now makes up a fast-growing field in the world of Mental Health. Derek Du Chesne of Better U, a mental health service in West Hollywood, shares how his team attempts to make psychedelic care safer, smarter and more accessible.
Mental health is finally getting the attention it deserves and as our understanding of it deepens, so does the range of tools available to support it. In recent years, psychedelic-assisted treatments like ketamine are gaining serious ground and a growing number of clinicians have turned to these as promising alternatives to more traditional methods. Enter Du Chesne, creator of Better U, with the goal of making ketamine therapy more accessible and personal. In our conversation, Du Chesne shares the mission behind Better U, the challenges faced by underserved communities and how his team is aiming to reshape the mental health landscape one patient at a time.
Can you share what Better U is all about?
I’m the founder and CEO of Better U. We’re a telemedicine-based alternative wellness platform, currently operating in 35 states. We primarily offer ketamine therapy for conditions like depression, anxiety, PTSD and suicidal ideation. We also provide services in sexual health, clinical weight loss and holistic psychiatry.
You’ve had your own experience with psychedelic therapy. Can you talk about how that journey inspired Better U?
Six years ago, I never imagined I’d be doing this. I had used psychedelics recreationally, but ketamine never interested me. I saw it as a horse tranquilizer nothing I’d ever take seriously.
I had been working in alternative health, specifically cannabinoids mainly on the supply chain side across several industries. In 2019, I traveled to about 40 countries for work and we raised around $40 million in capital. That year, my company made $85 million in revenue and was heading into a $1.2 billion acquisition. Personally, I was also about to get married. Within six weeks, both my career and my relationship unraveled. The company let me go just before my equity vested and I later found out my fiancée had been unfaithful while I was on the road.
Everything I had built my identity around collapsed. I spiraled into a deep depression, tried therapy, psychiatry, and antidepressants. None of it helped. Eventually, I became suicidal. A close friend intervened and brought me to a ketamine clinic. I was extremely skeptical, especially since a single session cost $1,600. But about 15 minutes into it, I felt like I could breathe again for the first time in months.
The treatment helped me separate from the constant, negative thought loops. It created space between me and my pain, helping me see that the things that happened didn’t define me. That clarity changed everything. I no longer felt like I had to carry shame or blame for what others had done. It gave me peace.
Shortly after, a friend suggested I get out of my environment. Everything in my home reminded me of the past. I went to The Bahamas for a reset: sun, exercise and healing. That period helped me recalibrate.
Months later, I was invited to Stanford by a friend whose sister leads epidemiology there. At dinner, I met someone involved in psychedelic research. I shared my experience and he invited me to visit their depression clinic and psychedelic research lab. That’s when I realized the transformative potential of these therapies. I sat with hospice patients receiving psychedelic treatments. People from all walks of life have similar, profound responses. It was incredibly moving.
That’s when I started thinking: how do we make this affordable and accessible? My first ketamine session was powerful, but afterward, there was no follow-up, just a “see you next week.” It felt transactional. I wanted to build something more thoughtful, especially for people like those in my small hometown in Wisconsin where mental health care is rare and stigma is high.
Better U was born from that idea.
Better U has facilitated over 230,000 sessions for around 18,000 patients nationwide. A large portion of your clients identify as LGBTQ. Why do you think ketamine therapy resonates so deeply with that community?
The LGBTQ community is incredibly diverse, and so are the challenges its members face, from gender dysphoria and identity struggles to rejection from family, friends, or society. That rejection often comes right at the moment someone begins living as their authentic self. The emotional toll can be devastating and in many cases, the suicide rates, especially among trans individuals, are alarmingly high.
Ketamine therapy creates space. It allows someone to step outside of the emotional chaos, the shame, fear, judgment and look at themselves without that mental noise. When you can separate your identity from the voices in your head or the reactions of others, there’s clarity. You begin to realize, “This pain isn’t about who I am, it’s about others’ inability to accept me.” That shift can be life-saving.
Many of our LGBTQ clients come to us after years of self-medicating with alcohol, drugs, or even unhealthy relationships. Others feel like they’ve hit a wall with traditional talk therapy. As we age, our brains get more set in their patterns. Ketamine disrupts those patterns. It can help people access a deeper level of understanding and healing, especially when other methods have stalled.
What’s powerful is that many patients don’t come in intending to stop drinking or using substances. They come for anxiety, depression, or suicidal thoughts. But after a few sessions, they’ll say, “I realize my drinking is tied to social anxiety,” or “I use because I feel like I have to numb myself to be accepted.” The therapy helps them see that those coping mechanisms aren’t serving them anymore.
We’re based in West Hollywood, so we’re deeply embedded in this community. In cases of suicide attempts, local hospitals like Cedars-Sinai often reach out to us because ketamine has become one of the most effective tools for treating suicidal ideation.
That said, it’s not a cure-all. If someone is abusing ketamine recreationally, we won’t treat them with it. It’s not safe or appropriate. But in a clinical setting, when properly dosed and supported with integration care, we’ve seen almost no cases of addiction. It can be a powerful tool for healing when used with intention.
Trauma-informed care is a term that gets used a lot in mental health these days, but what does it actually mean to you and how do you apply that framework at Better U?
To me, trauma-informed care means creating a system where every person interacting with a patient, from intake to integration, is trained to recognize, respect and respond to trauma. At Better U, we’ve built multiple layers of support to reflect that. While our welcome team handles basic screenings and eligibility, it’s our clinicians, integration therapists and success team who are most deeply trained in trauma-informed practices.
The unfortunate reality is that many ketamine clinics are founded by anesthesiologists—people who understand how to use the drug medically, but have little or no training in mental health. You can see it when you look at their teams: no psychotherapists, no psychiatrists, no trauma-informed staff. That’s dangerous, especially with a treatment that has the potential to surface deeply emotional material.
At Better U, we made sure to embed trauma-informed care into our clinical culture. Our doctors like Dr. Zaa Faul—a dual-board-certified addiction specialist and Army veteran—and Dr. Jamie Brooks, have deep expertise in both mental and physical health. Our success team, which supports patients after their sessions, is mostly made up of licensed therapists and professionals with years of experience in crisis care, psychedelic research and emotional integration.
Trauma-informed care also means learning how to hold space for people in distress. When I was the only person speaking to patients in our early days, I got yelled at, cussed out, blamed, not because patients were “bad” people, but because they were in pain. Maybe they hadn’t slept, or fasted before a session and were feeling raw. Maybe they were grieving or reliving trauma. You have to meet people where they are, understand that it’s not personal, and guide them toward healing without judgment. That’s where nonviolent communication becomes essential too. It’s a big part of how we train our staff.
Ultimately, it’s not just about delivering a treatment. It’s about helping people feel seen and safe enough to transform. And when you do that well, you get to witness incredible things, like someone processing deep grief or suicidal thoughts in a matter of weeks, instead of years. That’s the beauty of this work.
Let’s say I’m a potential patient who’s hesitant of undergoing ketamine therapy. What would you say to ease my mind?
Sure. First, I’d ask, have you ever had any experience with psychedelics?
[Then, I’d explain] most people who come to Better U, probably over 95%, have never had any experience with psychedelics. So it’s completely normal to feel anxious going into a first session and entering an altered state of consciousness. Especially if it’s unfamiliar.
I want to be transparent—our program isn’t a microdose. It’s a full, immersive experience.
That said, let me walk you through what the process actually looks like so you know what to expect.
After a consultation with a doctor to make sure this is a safe and appropriate treatment for you, you’ll receive a kit in the mail. That includes a blood pressure cuff, a journal, a “brain box,” and other tools to support your experience.
Then, before your first session, you’ll have a mandatory preparation meeting with one of our therapists. That’s where you can ask any remaining questions or talk through any lingering anxiety. You can even request a group session if you want to hear what others are feeling.
We also start very slowly. Your first dose is intentionally low — it won’t feel like a full psychedelic trip. It’ll feel more like a medication-enhanced meditation. It’s really just a way to help you dip your toe in and see how your body and mind respond before we increase the dose.
Is it safe?
Yes, incredibly safe, when done properly. Our protocols are built to prioritize your safety at every step. We’ve worked with thousands of patients and have seen incredibly low rates of any negative outcomes, especially when compared to traditional psychiatric medications.
And to be direct, while this work can be uncomfortable at times, it’s not always sunshine and rainbows, it’s also where the breakthroughs happen. This treatment acts like a mirror, helping you see what’s going on inside, but from a different, often clearer, perspective. And sometimes just that shift in perspective can change everything, from how you relate to yourself to how you engage with the world around you.
Where do you see Better U going in the near future, and how do you see it shaping the future of mental health?
Right now, one of our primary focuses is on insurance credentialing for all of our providers. Most of our patients come to us already on medications – antidepressants, benzodiazepines, Adderall, and so on—and as things currently stand, we can’t legally give them a plan to taper off or discontinue those medications.
So, let’s say someone goes through eight ketamine sessions with us and feels amazing, but they’re still on Xanax or an SSRI—we can’t formally help them get off of it. I think a huge issue in the U.S. right now is over-diagnosis and over-prescription. So by getting our doctors credentialed to accept insurance, including Medicare and Medicaid, we can create six month plans.
For example, to help patients reduce or discontinue medications that may no longer be serving them. At the very least, we want to help people lower their dosages to give themselves a fighting chance. Because right now, mental health care in this country is incredibly broken.
We’re also implementing AI. We’re about to launch a 24/7 companion app that provides continuous support. I think one of the reasons Alcoholics Anonymous has been so successful is the sponsor model. We’re building something similar: an AI “sponsor” or companion that can provide round-the-clock mental health and physical wellness support. Think of it as an AI therapist that works alongside the human element.
Looking further ahead, we’re also preparing for the future of MDMA-assisted therapy, psilocybin and other emerging treatments. There’s a lot coming and we’re positioning Better U to be at the forefront of it all.
Viewpoint
I’m a queer Iranian Jew. Why I stand with Israel during this conflict
‘Hands Off Iran’ movement is erasure, not solidarity

The sirens cut through the night, jolting me from sleep. My heart pounds as I lie in bed, listening to the explosions outside. I don’t have to run — my Airbnb bedroom is a “mamad,” a reinforced bomb shelter built into the apartment. Though the windows are sealed, I can feel the building shake with each blast. This is my reality now.
I arrived in Tel Aviv just before the escalation with a delegation of North American LGBTQ leaders. We came to stand in solidarity with Israel’s LGBTQ community, which has increasingly been isolated by the global queer movement. After the delegation’s five-day mission, I had planned to stay an extra week. But on my first night here, the war broke out.
Despite the fear and chaos, I’m proud to be here. While I’m not a permanent resident of Israel — I live in Los Angeles, home to the largest Iranian Jewish community in the U.S. — I feel like I’m exactly where I’m meant to be. I work in both Iranian and Jewish advocacy spaces, and being here during this pivotal moment is an act of presence, of witness, and of resistance.
The adrenaline of seeing Israel strike back against the IRGC gave way to the sobering realization: I am in a war zone. But I know I’m safer here than I would be in many other places — because Israel protects its people. With shelters. With missile interceptors. With warnings. With a government that values civilian life.
In Iran, people don’t have that. The regime in Iran — and I use that term deliberately, because the regime is not the people — cut off internet access to prevent civilians from receiving IDF warnings before strikes. They wanted maximum casualties. They wanted suffering. They wanted images to manipulate. The same regime that imprisons, tortures, and executes LGBTQ people. The same regime that stripped my family, and millions of others, of their home.
So, when I heard the same anti-Israel activists who have spent the past 20 months calling to “globalize the Intifada” — a clear genocidal chant — adopt the new catchphrase “Hands Off Iran,” my heart sank. This is not solidarity — it’s erasure. These people defend the very regime that forced my parents to flee, tearing our family apart.
Romanticizing the Iranian regime with protest signs and slogans isn’t just tone-deaf. It’s prioritizing aesthetics over truth, trend over substance, and optics over people. It’s especially painful when I see it coming from my LGBTQ peers.
Growing up queer in the Iranian Jewish community during the ’80s and ’90s wasn’t easy. It was LGBTQ spaces that taught me how to stand tall in my truth — how to live authentically and reject shame. But now, those same spaces often turn their backs on me because I’m a Zionist, a widely misunderstood movement which simply calls for Jewish self-determination.
The hypocrisy of the current anti-Israel rhetoric is glaring. The “Hands Off Iran” movement is misguided, providing cover for a regime that tortures its citizens. Yet these activists were nowhere to be found during critical moments like the 2022 “Woman, Life, Freedom” uprisings, when Iranian women risked their lives burning their hijabs in protest. After Mahsa Amini was murdered simply for showing a little hair, those cheering “queers for Palestine” said nothing. This silence in the face of tyranny is not progressive — it’s dangerous.
For me, this conflict is not theoretical — it’s personal. I’ve witnessed firsthand how the Iranian regime targets LGBTQ people, religious minorities, and women. In Israel, I’m free to be who I am — a queer Iranian Jew. If we fail to stand with Israel, we fail to protect the values of freedom, human rights, and dignity. Israel is more than just a country — it’s a refuge for people like me, and it must remain that way.
As I write this, a fragile ceasefire is in place. But even with the quiet, the clarity remains. Israel is more than just a nation. It’s a refuge. And it’s worth standing up for — not because it’s flawless, but because it’s real. And because without it, people like me — queer, Iranian, Jewish — would have nowhere to turn.
Matthew Nouriel is a digital producer at the Tel Aviv Institute, Community Engagement Director at JIMENA, and a queer Iranian Jewish activist. He lives in Los Angeles.
Opinions
Pride and Protests: A weekend full of division
Amid more upcoming raids and protests, we will have to learn when to act, how to react and when to find pockets of joy to celebrate in, because those moments are also acts of resistance

While many Angelenos celebrated the 55th annual L.A. Pride and mainstream news outlets like ABC7 and FOX11 news covered the celebrations, the reality for many other Angelenos involved tear gas, rubber bullets and breaking news coverage from community-led outlets like CALÓ News.
If we were to take a step back into the history of Pride, we would be angered by the amount of violence and pain that led to the protests on the dawn of June 28, 1969. The Stonewall uprising took place as a result of police raids at the now-infamous Stonewall Inn on Christopher Street in New York City. The night that has gone down in history as a canon event for queer and trans life began when police raided the Stonewall Inn and arrested multiple people. The arrests and the police brutality involved, led to an uprising that lasted a total of six days.
Marsha P. Johnson and Sylvia Rivera were credited as being the first people in that historical moment to start the movement we now know and celebrate as Pride. They were Black and brown, people who transformed our notions of fear and action, modeling the mantra that we must act in order to not live in fear. The people at the Stonewall Inn on that night in June all those years ago, and all of the queer and trans people now, have something deeply unsettling in common.
We both live in a constant state of fear and anxiety.
We live in such a major state of fear that anxiety, depression and other mental health issues — including substance abuse disorders — tend to be particularly prevalent in the LGBTQ community. According to Mass Gen, the U.S. is facing a mental health crisis, with nearly 40% of the LGBTQ population in the U.S. reported experiencing mental illness last year, a figure of around 5.8 million people.
Pride began as the very type of protest that went on this past weekend over the U.S. Immigration Customs Enforcement (ICE) raids, where people have been taken into custody, reporters shot with rubber bullets and tear-gassed, and where union president David Huerta was taken into custody and charged with alleged federal conspiracy charges.
Over the weekend, I celebrated Pride. I admittedly celebrated being queer, while my other communities experienced fear in the face of arrests, tear gas to the eyes and baton blows to the head. It was an internal battle I was not prepared for and a real battle on the streets I was not ready to experience. It made me feel weak and more than anything, I felt tired. I felt scared and I felt like I was not prepared for what was to come from these arrests and this violence.
I am a proud child of immigrants. My mother is Colombian and migrated here in the early 80s, settling down in West L.A and building a life with children, houses and her religious community.
My father migrated here in the mid-to-late 80’s from Mexico, where he and his family were hardworking farmers. He has worked at his job, without rest, for over 35 years. He rose up the ranks from line worker to general manager. He does not miss work. He follows every rule and he is never late. Both are documented, but only because of luck and the ease of getting papers back when there weren’t so many bureaucratic steps to gaining citizenship or a green card legally.
My parents and their extended family are proof of a now-distant American Dream, one in which we gain status, we become homeowners and business owners, have children and send them off to college to learn things that our parents can’t even imagine.
Though they did the best they could, my parents had other challenges and barriers to their success. So I worked hard in order to succeed for them. I did it for all of the people in my communities. I did it to raise the statistics on Latinx people, LGBTQ people and former foster youth who go on to college despite the odds and get higher education degrees.
My road to where I am now was paved with uncertainty, food insecurity, homelessness and many other factors that pushed and pulled me back. The analogy I can think of to accurately compare myself to is a catapult. I was pulled down with weights that were added on more and more, until one day I catapulted forward into the life I now have the privilege to live. Though I still struggle in many ways, it is the first time in my life that I am not in survival mode. It’s the first time in my life that I get to exist as a queer person who can enjoy life, build a friend group and establish deep connections with people. It’s also the first time I get to enjoy Pride as someone who is single and who has spent the past 18 months healing from my from my last relationship.
It was the first time in my life, as a lesbian who’s been out for over a decade, that I truly planned to enjoy Pride with my groups of friends.
While I was there this weekend, my internal battle began and I felt torn between celebrating my life and my queerness and covering the ICE raid protests happening not too far from Sunset Blvd.
What I didn’t expect was to see so many other people at Pride, completely oblivious and completely disconnected from the history of Pride, instead glorifying corporate brands and companies that have remained silent over LGBTQ issues, while others have gone as far as rolling back their Diversity, Equity and Inclusion initiatives.
If Marsha P. Johnson or Sylvia Rivera were there at that moment, they would have convinced us to merge our Pride celebration with the protests. They would have rallied us all to join forces, and in the spirit of Pride, we would have marched for our immigrant community members, fighting for their right to due process.
I’m not sure if I made the right decision or not, but the next 60 days will say a lot about every single one of us. We will have to learn when to act, how to react and when to find pockets of joy to celebrate in, because those moments are also acts of resistance.
The Trump administration vowed to strip away rights and has made it their mission to incite violence, fear and anxiety among all working class, BIPOC and LGBTQ people, so it is important, now more than ever, to unite and show up for each other, whether you’re at a Pride celebration or a protest.
The next 60 days will raise our anxiety and fear, but we must remember to also take breaks, celebrate wins, relish in community, hug your loved ones and use whatever amount of privilege that you have, to show up for the communities that are hurting the most in these moments.
Juneteenth is also coming up soon and I hope to see more of us rally around our Black brothers, sisters and siblings, to not only fight for our rights, but to continue celebrating ourselves and each other.
In the words of Marsha P. Johnson: “There is no pride for some of us, without liberation for all of us.”
California
New California trans athlete policy creating ‘co-winners’ is a crock
You didn’t misread that. Hernandez shared the podium with ‘co-winners’

A lot happened at last weekend’s high school state track and field championship meet in
Clovis, Calif. Parents of cisgender student-athletes booed the one and only transgender
girl competing. Police and security officers showed up in large numbers to keep
protestors apart and safeguard the competitors. Police made an arrest outside the
stadium after a demonstrator brandishing a transgender pride flag allegedly assaulted a
man described as a conservative activist and caused damage to his vehicle.
The trans student — 16-year-old AB Hernandez — finished a winner. But she wasn’t “the” winner.
As CBS News reported, “Hernandez took home first place medals in both high jump and
triple jump and she placed second in the long jump event. Following a rule change by
the California Interscholastic Federation, a co-winner was named in each of the three
events in which Hernandez placed.”
You didn’t misread that. Hernandez shared the podium with “co-winners.”
As the Blade reported last week, the CIF introduced a new “pilot entry process” that for
the first time, allowed judges to score trans athletes separately from cisgender
competitors, so there were three winners in every event: a cisgender male winner, a
cisgender female winner and a trans student-athlete winner.
The new policy was announced hours after President Donald Trump threatened to pull
“large scale federal funding” from the state if officials allowed trans athletes to compete
according to their gender identity.
Despite the policy change, the U.S. Department of Justice announced on social
media it was investigating State Attorney General Rob Bonta, State Superintendent of
Public Instruction Tony Thurmond, the Jurupa Unified School District, and the CIF for
potential violations of Title IX, as the Blade reported.
So what happens now? As KXTV reported, President Trump issued another threat to
pull funding on Monday in a post to his Truth Social account, not naming Hernandez but
labeling her “a biological male” and using his favorite derogatory nickname for
California’s Democratic Gov. Gavin Newsom.
“A Biological Male competed in California Girls State Finals, WINNING BIG, despite the
fact that they were warned by me not to do so. As Governor Gavin Newscum fully
understands, large scale fines will be imposed!!!”
Now, the pundits are weighing-in. Sara Pequeño wrote in USA Today how she was
encouraged to see Hernandez share the 2nd place podium with Brooke White and “put
their arms around each other.”
“They’re setting an example for how all of us should treat our trans neighbors, i.e.,
treating them like human beings, not enemies,” she wrote.
As Pequeño noted, Save Women’s Sports, an anti-trans advocacy group, could only
identify five trans students in the entire United States who were competing on girls’
teams from kindergarten through grade 12 in 2023. “That group’s entire existence is to
hate trans athletes, and they found very little to hate,” she wrote.
According to the president of the NCAA, there are fewer than 10 student-athletes
who publicly identify as transgender out of the more than 500,000 competing at the
collegiate level.
Pequeño was not alone in finding joy in the rules change that brought cisgender and
transgender girls together on a podium, each of them a “co-winner.” So did self-
proclaimed “trans advocate” Cyd Zeigler.
He’s one of the co-founders of the LGBTQ+ sports site Outsports, who in 2023
infamously came close to endorsing Florida Republican Gov. Ron DeSantis for
president, only to offer his regrets, following a backlash from readers. Zeigler penned an
op-ed Wednesday originally titled “California trans athlete policy is something everyone
can embrace.”
“Everyone?” Not this sports editor.
He called the new CIF policy “the best possible path in 2025 to trans participation in
sports.”
In celebrating this change, Zeigler also trashed “goal-post-moving trans advocates” and
policies in California and Connecticut that allow “a trans girl to run in boys track meets
and, without a medical transition, later compete in girls meets,” meaning high school
competitions. “That’s bad policy,” declared Zeigler without evidence.
That policy in Connecticut has stood since 2011 and is enshrined in state law, and so far
has withstood legal challenges once again being heard in federal court.
Outsports at some point changed the headline of his screed to “New California trans
athlete policy is something we can embrace” and apparently made another significant
choice: Despite quoting the outlet’s one and only remaining transgender contributor,
Karleigh Webb, who opposes the rules change, Zeigler did not mention her by name.
Why?
In an article published before the championship, Webb wrote: “If AB Hernandez wins,
why should she have to share the spoils with someone else if’s not a tie? That’s what
professional transphobes like Jennifer Sey and Riley Gaines try to sell. Awarding a
duplicate medal gives their nonsense credence to the detriment of the sport and the
athletes.”
Webb is right. Zeigler and the CIF and Gov. Newsom are wrong. You either win, or you
lose, or if you prefer, you come in second, third, whatever. But “co-winners?”
That’s a crock.
Imagine if the Dodgers and Yankees shared the World Series trophy. Why shouldn’t the
49ers also win the Super Bowl alongside the Chiefs? Maybe Kamala Harris should be
declared a “co-winner” of last November’s election?
Personally, I’m glad to see Hernandez embraced by her cisgender peers. I’m relieved to
know that crowds cheering these amazing girls last weekend drowned out the hecklers
who showed up to boo a child. I’m encouraged that even if she had to share the win,
Hernandez was given her rightful place among the teens competing and proved she
was not only worthy of competing but did not win in every event.
So, she’s hardly “unbeatable.” Most trans athletes actually lose, as Zeigler wrote almost
six years ago, back before he started echoing anti-trans inclusion activists Martina Navratilova, Renee Richards and Nancy Hogshead-Makar.
If he really thinks the CIF “co-winners” rule is going to silence anti-trans forces, I think
he’s going to be very surprised by Riley Gaines and her crowd.
While it’s easy for Zeigler to concede public opinion has shifted, he should know
better than to blame those who pushed for inclusion, when it’s clear that conservative
voices in media and politicians, like his, are the ones responsible for influencing that
move to reject trans women’s right to compete in women’s sports. It’s a pendulum swing
that in time will undoubtedly swing back, once the science proves that trans women and
girls don’t always win. In fact, researchers have already proven some trans athletes are
at a disadvantage compared to their cisgender competitors.
Just as Parker Molloy reported that a Republican-commissioned study on gender
affirming care in Utah actually found “that youth who received care before age 18 had
better outcomes, especially around depression, anxiety and suicidality. Hormonal
treatments were associated with positive mental health and psychosocial functioning
outcomes.”
I believe the science is on the side of transgender Americans. Americans love a
winner. Not a “co-winner.”
Opinions
Trump’s inhumanity won’t erase Andry Hernandez Romero, if we resist
Andry Hernández Romero’s case continues to be a violent reminder that we must rise up and resist
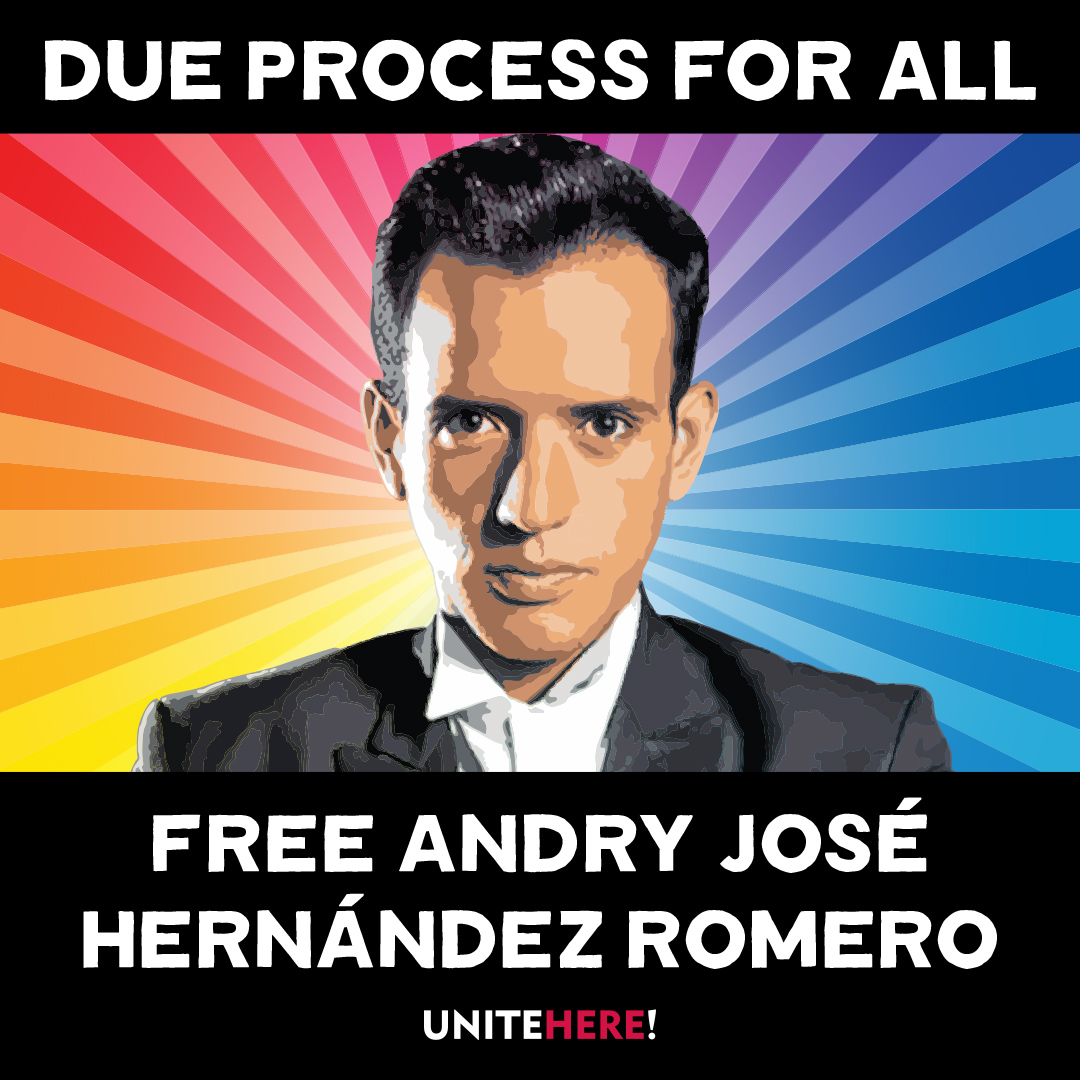
Editor’s Note: Since this article was first published, more information on Andry’s case has become available.
UPDATE: On June 4, a federal judge ruled in favor of the ACLU and Democracy Forward in J.G.G. v. Trump, in which deported gay stylist Andry José Hernández Romero is one of the lead plaintiffs. Describing the Venezuelan deportees’ situation as Kafkaesque, Judge James E. Boasberg said the plaintiffs would likely prevail in their complaint about being denied due process, the New York Times reported. Trump officials, Boasberg wrote in his 69-page ruling, “spirited away planeloads of people before any such challenge could be made. And now, significant evidence has come to light indicating that many of those currently entombed in CECOT have no connection to the gang and thus languish in a foreign prison on flimsy, even frivolous, accusations.”
“Absent this relief,” the judge wrote, “the government could snatch anyone off the street, turn him over to a foreign country and then effectively foreclose any corrective course of action.” He ordered the Trump administration to give the deportees the due process they have been denied.
On Friday, June 6, Rep. Pramila Jayapal (WA-07), Ranking Member of the Immigration Integrity, Security, and Enforcement Subcommittee, will host a shadow hearing Kidnapped and Disappeared: Trump’s Lawless Third Country Disappearances at which Andry’s attorney Lindsay Toczylowski will testify.
The juxtaposition is morally excruciating. The very air in West Hollywood is electric with
queer joy and the excitement of WeHo Pride, but it’s more than a celebration of our ongoing
movement for liberation and equality. We’ve been waiting for a moment to exhale and
stop the clamor of the Trump horror show.
What can we do to stop this overwhelming dictatorship campaign that is gleefully
enforcing Project 2025 through a deluge of cruel Executive Orders, demonizing and
erasing anything under Diversity, Equity and Inclusion initiatives and LGBTQ while dispatching masked ICE agents to snatch anyone Trump’s White Supremacist terrorist administration tags for deportation.
Among those swept up in Trump’s frenetic crusade is Andry Hernandez Romero, a 32-
year-old gay hair stylist and makeup artist who fled harassment and threats of violence in Venezuela in May 2024, after speaking out against authoritarian dictator Nicolás Maduro. After navigating the complex app designed to streamline the byzantine U.S. lawful entry process, last August Romero faced a U.S. border official in San Diego. With no criminal history, he demonstrated a “credible fear of persecution” to proceed with an asylum case.
Imagine what Romero felt — so close to freedom, to opportunity, to unabashed queer joy.
Then came that Trumpian twist.
During a physical exam, officials fixated on Romero tattoos of crowns with the words “Mom” and “Dad.” The agent apparently assumed that Venezuelan gangs accept gays because he suspected Andry had gang affiliations and does not fact check because Tren de Aragua does not use crown tattoos for gang identification.
Romero landed in detention awaiting his asylum court date. But one week before the
March 13 hearing in San Diego, Romero was abruptly transferred to a facility in South
Texas, resulting in his absence in court. The hearing was postponed to March 17 when
the immigration judge again asked where Romero was.
“He was removed to El Salvador….we just found out today,” the ICE lawyer replied. The judge questioned the legality of Romero’s deportation without a removal order.
On March 14, Trump invoked the Alien Enemies Act — a 1798 law used during a
declared war — to target immigrants as government “enemies” who had “infiltrated”
America. Secretly, ICE deported Romero and 137 other Venezuelans to El Salvador’s
notorious Terrorism Confinement Center, with Trump paying dictator President Nayib
Bukele to incarcerate the kidnapped immigrants.
The world watched as Andry and his shackled fellow prisoners were displayed on TV
brutally forced off the plane and forced to kneel as agents roughly shaved their heads.
TIME Magazine photographer Philip Holsinger reported that Romero was being slapped while crying out for his mother, “I’m not a gang member. I’m gay. I’m a stylist.”
Trump called the Venezuelans “rapists,” “savages,” “monsters” and “the worst of the
worst,” claiming they were thoroughly vetted. But ProPublica reviewed each case of the
Venezuelan deportees and reported that the Trump administration knew that “the vast
majority” of the 238 Venezuelan immigrants ”had not been convicted of crimes in the
United States before it labeled them as terrorists and deported them, according to U.S.
Department of Homeland Security data that has not been previously reported.”
Lee Gelernt, the American Civil Liberties Union’s lead attorney fighting the deportations,
told ProPublica that the removals amounted to a “’blatant violation of the most
fundamental due process principles” and subjected the deportees to life imprisonment.
There have been numerous attempts to look for a humanitarian bone in the Trump
administration’s body politic, most notably gay immigrant Rep. Robert Garcia’s heated
exchange with Homeland Security Secretary Kristi Noem during a May 14 congressional hearing. Garcia (D-Long Beach) went to El Salvador for a welfare check
but was denied access to Romero.
“He has had no access to lawyers or family since he has been taken over a month now,”
Garcia told Noem. “His mother just wants to know if he is alive.”
“I don’t know the specifics of this individual case. This individual is in El Salvador and
the appeal would be best made to the president and to the government of El Salvador
on this,” replied Noem.
Garcia pushed back.
“You and the president have the ability to check if Andry is alive and is
not being harmed. Would you commit to at least asking El Salvador if he is alive?”
Nope.
“This is a question that’s best asked to the president and government of El
Salvador,” she said.
Noem’s callous disregard for life and suffering is unsurprising. The former governor of
South Dakota blithely noted in her political memoir that she shot and killed her 14-
month-old dog Cricket when the puppy misbehaved. “I hated that dog,” Noem wrote.
She also shot a goat she didn’t like.
“In neither case did Noem show any doubt or remorse; quite the contrary, she sought to
cast her action as a signifier of tough-minded realism that would burnish her appeal as a
politician from a rural community,” wrote Sara Amundson, president of the Humane
Society Legislative Fund.
So if Noem thinks callousness is cool, imagine how she feels about someone she might
deem as sensetive?
“Under the Constitution, every single person has a right to due process, and that means
they have a right to notification of any allegations the government is making against
them and a right to go into court and prove that those allegations are wrong if that’s the
case,” Lindsay Toczylowski, President of the Los Angeles-based Immigrant Defenders
Law Center who is representing Romero pro bono, told NBC News San Diego April 11.
“In Andry’s case, the government never gave us that opportunity. In fact, they didn’t even
bring him to court, and they have forcefully sent him to El Salvador without ever giving
us any notice or without telling us the way that we could appeal their decision.”
On May 27, Immigration Judge Paula Dixon granted a U.S. Dept of Homeland Security motion to dismiss asylum proceedings for Romero scheduled for the following day.
“We should all be incredibly alarmed at what has happened in Andry’s case. The idea
that the government can disappear you because of your tattoos, and never even
give you a day in court, should send a chill down the spine of every American. If this can
happen to Andry, it can happen to any one of us,” said Toczylowski.
Andry’s life depends on us holding the Trump administration accountable for what they
have done to him,” Toczylowski said. “We will continue to fight until Andry is safe and
free.”
Romero is a lead plaintiff in the American Civil Liberties Union’s and Democracy Forward’s J.G.G. v. Trump case in which Romero’s friend and mother gave statements that are now evidence saying Romero “was persecuted both for his sexual orientation and for his refusal to promote government propaganda” while working as a makeup artist at the TV network in Caracas, according to CNN.
But Project 2025 booster Kevin D. Roberts doesn’t care, having ordered the Trump
administration to delete “the terms sexual orientation and gender identity….out of every
federal rule, agency regulation, contract, grant, regulation, and piece of legislation that
exists.”
So do Trumpland judges care about the raison d’etre for asylum or is that too DEI?
NBC News reported that Romero’s dismissal order “allowed for the possibility that the
case be reopened if Hernandez returns to the U.S.”
That’s why we the people, must rise up and resist.
“As the son and grandson of Japanese Americans who were rounded up and forced into
camps without due process, I know all too well that Andry is not the first person to be
unjustly taken by the government,” says out Rep. Mark Takano (CA-39), Chair of the Congressional Equality Caucus. “Every American should be alarmed by how openly the
Trump Administration is taking people off the street and locking them away in a foreign
prison without so much as a day in court — all because of their tattoos. This fight is not
over yet, but every day it drags on puts Andry and others’ lives in danger. I stand with
Andry, his family, his lawyers, and our Constitution in rebuking President Trump’s cruel
and illegal attacks, and hope that justice is swiftly served.”
Longtime activist Cleve Jones urges all LGBTQ people and allies to take action.
“We don’t know if he’s dead or alive,” Cleve says. “I look at [Romero] and he’s like my little
gay brother who is now in this terrible situation where he — if he is still alive — is probably
being subjected to horrendous brutality on a daily basis.”
But Cleve is also angry at the lack of response to this urgently important case.
“If you want to be intersectional and not just quack about it, look at this case,” Cleve
says. “This young man stands at the intersection of our fight for LGBT equality, for
immigrant rights, and for due process under law.”
San Francisco Pride and New York City Pride rejected his request to name Andry an
honorary Grand Marshal. But, Cleve says, “I’m happy that a number of pride
celebrations have done that. Others have stepped up and are organizing fundraisers. I
see there’s one coming up in New York. But everybody should be talking about Andre.
Free Andre. Free Andre. It’s so important!”
Please note: To support Romero’s case and others like it, the Immigrant Defenders Law Center is selling a T-shirt that says “Asylum is a Human Right, found here.“
Community Perspectives
‘Protect the dolls’: The viral t-shirt that sparked a movement
The shirt’s message and its impact have turned this moment into a cultural flashpoint

In February 2025, American designer Conner Ives closed his fall and winter show at London Fashion Week with a striking message — not spoken, but worn.
He walked the runway in a T-shirt reading “Protect the Dolls” a phrase that has since gone viral and ignited a wave of support for trans rights around the world. The shirt, now worn by celebrities and activists alike, has become more than a fashion statement — it’s a declaration of solidarity, a tribute to trans dignity and trans rights and a call to action.
“The night before the show, my team and I were sitting around throwing around slogans that we would put on a shirt, which led to Protect the Dolls,” explained Conner Ives in an interview with Trans Lifeline.
The phrase, simple yet powerful, was designed to cut through the noise.
“Maybe the reason that the catchphrase caught on,” said Ives. “Is that rather than coming in with testimonials or facts or percentages… this was maybe a way to simplify down the message to something that could just be said in three words.”
The word “doll” has deep roots in LGBTQ culture, tracing back to the 60s and 70s ballroom scene created by Black and Latino, trans and queer communities. In a world that routinely rejected them, calling each other “doll” was an act of affirmation — a way to celebrate beauty, softness and survival. The term of endearment became a symbol of sisterhood and resistance — a coded language of care in hostile environments. By calling each other dolls, we affirm our beauty, our care and our worth. Like the way societies throughout human civilization have treated cherished dolls — with love, nurture, and tenderness — the term has become a powerful emblem of resistance, sisterhood and self-love.
Today, as trans rights face increasing attacks both in the U.S. and around the world, remembering this legacy feels more urgent than ever. Earlier this year, President Donald Trump, now in his second term, signed multiple executive orders severely restricting transgender rights. Meanwhile, in the U.K., the Supreme Court’s redefinition of “woman” has excluded trans women from key legal protections, marking a major setback for equality. As Ives reflected, “It feels like we are sometimes living in two alternate realities simultaneously… the alternate reality where we have the people that we choose around us, and then the one filled with political theater and hysteria.” In this climate, “Protect the Dolls” is more than a slogan — it’s a rallying cry to defend our rights, affirm our dignity and celebrate the communities we build together.
The shirt’s message and its impact have turned this moment into a cultural flashpoint. Celebrities across fashion, film, music, and social media have rallied around the design, turning their platforms into megaphones for its mission. Pedro Pascal wore it to his 50th birthday party alongside DJ Honey Dijon and again at the European premiere of “Thunderbolts (2025).”
Troye Sivan wore it on stage during Charli XCX’s Coachella 2025 set, where they performed “Talk Talk” together — a redux of their joint tour last year. He later posted a photo wearing the shirt alongside Lorde, Charli XCX and Billie Eilish, further cementing its status as an iconic fashion moment. Other high-profile supporters include Addison Rae, Tilda Swinton, Haider Ackermann, Emma Brooks, bbno$, Lisa Rinna and Camille Charriere — all of whom have proudly shared it on social media. Their posts have helped catapult the shirt into the global spotlight, transforming it into both a fundraiser and a visual rallying cry.
The shirt which sells for £75 (about $99 USD), is available through Ives’s website, with 100% of the proceeds benefiting Trans Lifeline — a nonprofit organization run by and for trans people. Since its launch, over 5,000 shirts have been sold, helping to fund Trans Lifeline’s critical services, including its peer-led crisis hotline and its micro-grants program, which has already distributed over a million dollars directly to trans people.
“I think maybe what really sealed the deal for me was reading the quip somewhere where this is a trans-led U.S.-based charity benefiting trans people,” said Ives.
“I’m not the one picking up the phone helping these people or answering the phones. I think that was really why I wanted that to go where it was going,” he emphasized.
He also emphasized the importance of transparency: “When people say $100 for a T-shirt is a lot, we break down the costs for them. We show them how we’re using organic cotton, fair trade environments, reputable factories—and that over two-thirds of proceeds are going to charity.” Ives even encourages critics to take action however they can: “If the shirt isn’t accessible for you, we tell people: make your own, and donate whatever you can directly to Trans Lifeline.”
What started as a closing runway moment has become a movement. “It feels now like it’s turned into something bigger than just a T-shirt,” Ives reflected. “It’s become a universal concept that is for the people as well. We don’t own that phrase.” In fact, when asked about trademarking Protect the Dolls, Ives responded, “Honestly no, because it’s not mine to own.”
“Protect the Dolls” is more than a fashion statement — it’s a declaration of solidarity and a call to action. Every shirt worn is a stand against the forces that seek to erase us, a tangible investment in a future where trans people not only survive, but thrive. It’s a reminder that our lives, our joy, and our futures are worth fighting for.
Because in the face of systemic violence, we protect each other.
We protect the dolls.
Community Perspectives
How a promoter brought Middle East Nights to WeHo Gay Bars
Mas is interested in challenging assumptions in the West about sexuality in the Middle East
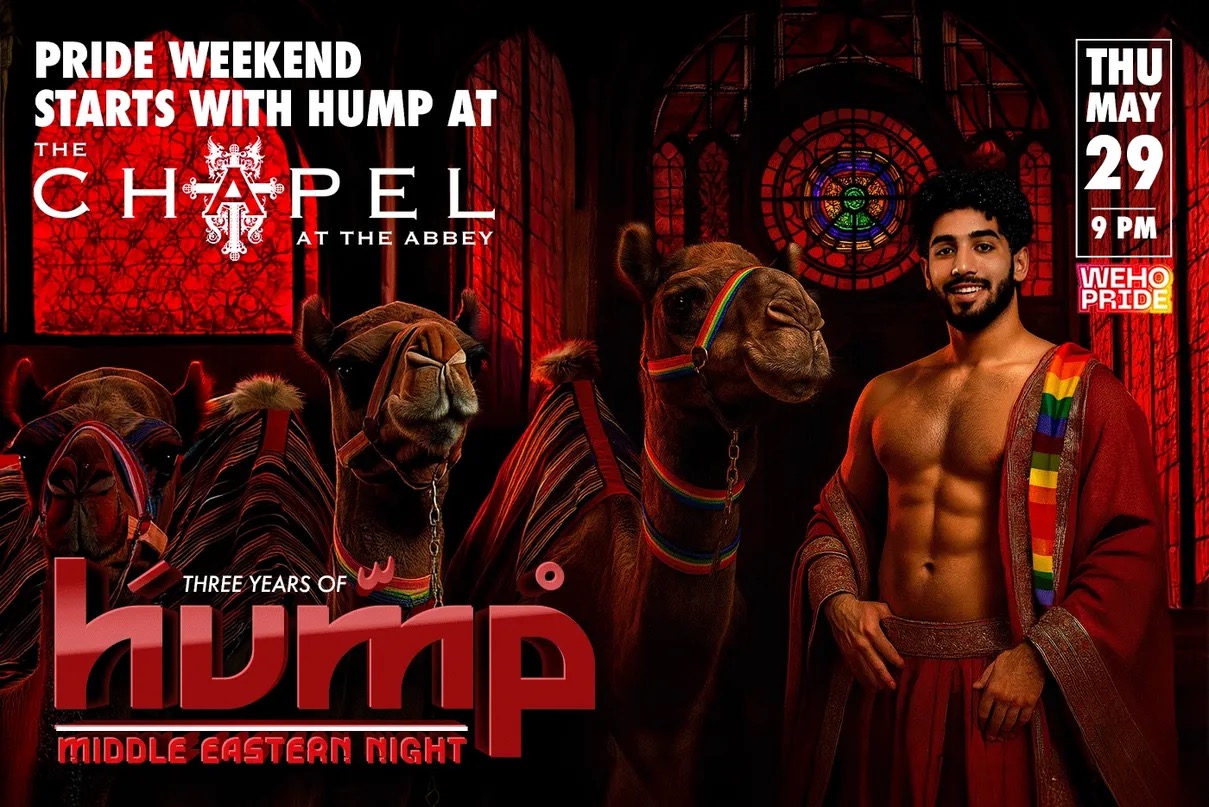
Mas never meant to become a club promoter. He’s a broad man with a neat beard and twinkling eyes above a grin. After studying marketing and management in the U.S., he returned to the Middle East to help a Dubai company open luxury movie theaters across the region — including the first ever movie theater in Saudi Arabia.
When Covid-19 hit, theaters shuttered and the Lebanese economy crashed. Banks locked people’s money and so, starting over with nothing, he returned to Los Angeles, where he crashed on a friend’s couch for three months.
Ingenuity makes strange bedfellows. When Micky’s in WeHo offered Mas a bartending gig, he pitched the idea of taking over their marketing campaigns instead. Months later, after helping to get the word out about all sorts of different events and evenings, the club asked him if he’d consider hosting a night.
Mas is interested in challenging assumptions in the West about sexuality in the Middle East by hosting this night in the gay-famous WeHo community.
At the time, Mas says, there were no events for the gay Middle Eastern community in L.A., which includes Arabs, Persians and Armenians. The only other gay, Middle Eastern-oriented club was Club Nur, which is now permanently closed. So he thought of hosting his own.
“I wanted to create a space for us to listen to our music,” said Mas. “A place for us to be homesick.”
As a new promoter, the club didn’t offer Mas a weekend, but rather a Wednesday night, which are notoriously difficult to sell. But the day gave Mas the name for his first foray into nightlife.
“They already call it hump day,” he said.
The associations: camels and being horny.
“Save a Camel, Hump a Habibi,” says the screen at the bar, over an image of a shirtless man surrounded by decorative lamps. “Habibi,” is a word in Arabic without an easy translation. The most direct is, “beloved,” or “my dear,” but the part that defies translation is how it means both “friend” and “lover.”
For the first Hump event, the team brought a real live camel to West Hollywood to stand out in front of Micky’s as a photo op.
“To this day that’s what’s remembered,” he said.
People for the Ethical Treatment of Animals (PETA) got wind of what was happening and was not pleased — but Mas explains with an eye roll, that the camel was there for one hour, on an off night, with two trainers and was well looked after.
Mas then spoke about the club promotion politics of that night.
“I was a closeted college student in Louisiana when 9/11 happened,” he said, sharing how his white American friends ran errands for him in the days following the attacks so he wouldn’t run the risk of harassment just for leaving the apartment.
“I still get searched in every airport,” he laughed.
In 2008, he went on America’s Got Talent to perform belly dancing. During his audition, he told the panel that he was there to show the peaceful side of the Middle East and a producer came to him afterward, thanked him for his bravery, and told him that unfortunately they would have to cut his segment from the show for venturing into politics.
“People assume the West is better for gays, but that’s not always true,” he said. “The first experience of homophobia I remember, coming from Lebanon, was while my family was on vacation in Italy.”
“There were five gay clubs in Lebanon growing up,” said Mas. “They were more hidden than here, but they were there.”
He recalls that in Dubai, gay parties happened all the time, but the addresses would be released last-minute to prevent them from being shut down — much like LA’s thriving queer warehouse party scene. People will always find a way.
“In Lebanon, growing up, there was not one type of music.” Lebanon is a crossroads of culture, and influences from Europe and the Middle East mingled freely. “You’d hear English, Spanish, French, and Turkish, even just in how people greeted each other in the street.”
The mix of tunes at Hump parties reflects this vibrant music scene.
I attended Hump at Chapel at The Abbey in March, and the Persian holiday of Nowruz, the new year and start of spring.
“Tonight we’re celebrating the Persian people,” said Mas enthusiastically.
His framework is based on the question: who is being celebrated?
It’s a mixed crowd, and the music oscillates between American pop hits and Persian pop classics. “This one has 3 million Shazams,” exclaimed the similarly clueless white boy next to me when we look up the song that’s playing — which has inspired an eruption of passionate singing-along from the middle of the dance floor. My friend Ruben, who’s from Guatemala, twirls another man through classic Salsa steps, to the Persian beat.
“I don’t know a word, but it still makes me move my hips,” he laughed.
I was pleasantly surprised to find another friend, Ameed, working at the door. His social media feed is a continual anguished cry for his native Palestine, but here he sports a broad grin under his keffiyeh, welcoming people in.
“I never thought something like this could exist,” he said. “I was nervous my first time coming,” Ameed explains how coming out as gay to his family led him to take a step back from his own culture, even to see it as bad or bullying. “Every gay Arab guy has some sort of trauma,” he says. “But here I get to enjoy the parts of my culture I enjoy, while still feeling safe — and I get to meet other people in the same boat.”
When Mas talked about making a space “to be homesick,” I had taken it literally, imagining folks far from where they grew up longing for that homeland. Speaking with Ameed a new meaning dawns on me — the way we are homesick for parts of ourselves that we lose in coming out, or even just in growing up. West Hollywood nightlife is all about selling a fantasy. The fantasy here is of a self-aware person’s internal multitudes can be, even just for an evening, in harmony.
Sometimes that’s just a fantasy. Ameed, who says he works a boring, normal job, offered to staff the door after his last experience where he complimented a doorman on their keffiyeh, and the doorman didn’t know what he was talking about.
“Oh this? They just told me to put it on,” he said.
It’s always a fine line between celebration and appropriation.
Reflecting on how that night was a model queer utopia, I wonder if there’d be enough actual gogos from the Middle East to staff a night like that. Probably not.
The crowd is out in force by 11pm, but, classic Thursday, starts to thin after midnight. I was surprised by the number of women out, seemingly supporting the gay men in their lives.
While Hump started as a part time endeavor, Mas’s production team now puts on a slew of gay nights at various bars, including Barbearians (think lots of fur and leather, a play on the erotics of “savagery”) as well as, Steam, a bathhouse-themed night in which guests are encouraged to wear only a towel at the bar. While not specifically Middle Eastern, these nights have the fingerprints of their progenitor, from the music played to, at Steam — a Hookah station where guests can smoke water pipes outdoors and send up smoke like the steam at a bathhouse.
These parties have grown, now touring other cities and even bringing a float to WeHo Pride complete with a flying carpet and gay influencers from Iran, Tunisia, and Iraq. Barbearians, now entering its second year, recently hosted its first Mr. Barbearian competition, which will send the winner, Dé Hanno, to represent the event at Mr. International Leather in Chicago. There’s also intercultural collaborations, like Yalla Papi, a Middle Eastern and Latino night that blends the music of both cultures.
“Latinos move their hips side to side, Arabs move them up and down,” said Mas cheekily.
Mas stated that his goal is to foster a sense of cosmopolitanism and inclusivity. Hump and its progeny provide a safe space for queer Middle Eastern men and their allies to express their sexuality, but also create a meeting ground on their “home turf,” that challenges cultural conceptions both internally and externally.
Commentary
From pride to policy, it’s time to build in WeHo
‘West Hollywood isn’t just coasting on its values—we’re acting on them’

By John M. Erickson, West Hollywood City Councilmember
West Hollywood has always stood as a beacon for LGBTQ people, for the
marginalized—for anyone chasing a place to be safe, seen, and supported. But that
promise is slipping away. If people can’t afford to live here, then West Hollywood becomes a symbol, not a sanctuary.
The housing crisis gripping Southern California is particularly acute in LGBTQ communities. Whether it’s trans women of color pushed into homelessness, queer youth aging out of foster care, or seniors on fixed incomes being priced out of the very neighborhoods they helped shape—our inability to build enough housing is deepening the inequality we claim to fight against. Our failure to build enough housing is not just a policy gap—it’s a moral one.
This isn’t theoretical. It’s personal.
As a gay man and a progressive policymaker, I know what it means to live at the intersection of identity and action. I carry the legacy of those who fought for a seat at the table—and the duty to do more than just sit there. Right now, that means confronting a housing system that’s failing the very people we claim to protect.
When West Hollywood became a city in 1984, we inherited density. We had walkable
neighborhoods, apartment buildings, and a diverse housing stock. But we froze. For 40
years, our zoning has barely moved.
In the last 25 years, WeHo has actually decreased in population. Meanwhile the number
of Americans who identify as LGBTQ+ has more than tripled in that same amount of
time. We haven’t kept up with demand, and we haven’t met the needs of the vulnerable
communities we claim to champion.
That’s about to change.
On Monday, May 5th, I’m introducing a sweeping housing reform package aimed at one
thing: making it easier, faster, and cheaper to build homes in West Hollywood. Not just
luxury condos—homes people can actually live in. That means slashing red tape. Cutting delays. Dismantling outdated rules that stall projects and drive up rents.
This isn’t about bulldozing neighborhoods or silencing community voices. It’s about
fixing a broken system—one built for a different era and completely out of step with the
urgency of now. It’s time to stop confusing progressive branding with progressive
outcomes. We need real reform: faster processes, smarter regulations, and yes—political courage.
Will this fix everything overnight? No. But it will send a clear message: West Hollywood
isn’t just coasting on its values—we’re acting on them.
Housing justice is LGBTQ+ justice. It’s racial justice, economic justice, and generational
justice. We don’t get to call ourselves a queer haven if only the rich and lucky can live
here. The West Hollywood of the future must make room for drag artists, Trader Joe’s
cashiers, trans youth, longtime renters—and anyone else trying to build a life with
dignity.
A city that flies the Pride flag can’t stand by while its most vulnerable residents are
priced out and pushed out. We owe the next generation more than just slogans and
rainbows. Let’s leave them keys.
Commentary
On Pope Francis, Opus Dei and ongoing religious intolerance

“Good Friday” set the stage for Saturday’s anti-Trump/MAGA “Hands Off” protests serving as a timely lead-in to binge-watching Alex Gibney’s two-part HBO political documentary, “The Dark Money Game” on Easter Sunday. In “Wealth of the Wicked,” nefarious Opus Dei —Svengali Leonard Leo strategically seduces politically disappointed Catholic Federalist Society billionaires into subsidizing a scheme to ‘pipeline’ malleable conservative judges to take over the Supreme Court and overturn reproductive rights.
A key victory for “Operation Higher Court” came in 2010 when SCOTUS ruled 5-4 in Citizens United v Federal Election Commission, that corporations and unions have the same First Amendment free political speech rights as individuals—as long as their unlimited cash donations go to 501 c(4)’s or Super PAC slush funds and not directly to candidates. Twelve years later, in 2022, they got their payoff with the overturning of Roe v Wade by Leo-promoted Catholic justices.
But Leo’s political conniving is not the only exploitation of moral corruption. The documentary exposes conservative Christians too.
Gibney’s anti-hero is a former rabid anti-abortion lobbyist named Rev. Robert Schenck. He tells of turning to a fellow conservative in Cleveland, Ohio after Trump won the Republican presidential nomination in 2016 and asking: “Are we really going to do this? We’re going to choose this man who’s inimical to everything we believe?” The other evangelical replied: “I don’t care how bad he is. He’s going to get us the court we need.’”
Schenck explains the unholy alliance between Christian conservatives and Big Business. “Whenever you talked about government regulation, the argument was eventually —‘these same characters who control my business are going to start trying to control your church. So, it’s in your best interests that we defang this monster’— and that brought a lot of religious conservatives over.”
And there’s this: “We have a little aphorism built on a Bible verse: ‘The wealth of the wicked is laid up for the righteous.’ So, yeah, let’s baptize the billionaires’ money. We can do that — and it eventually brought together this alliance.”
Schenck later reveals an intense epiphany that resulted in regret for how much harm he caused. Not so for Leo.
This is an excerpt from Gareth Gore’s comprehensive book Opus, for Rolling Stone Magazine:
“DURING THE DONALD TRUMP YEARS, conservatives — led by Leonard Leo — took control of the Supreme Court…. At one Federalist Society event, his good friend Supreme Court Justice Clarence Thomas jokingly referred to Leo as the third most powerful man in the world, presumably behind the pope and the president of the United States.”
On Monday morning, Pope Francis died. I liked this pope, compared to the others. I covered Creating Change during the AIDS crisis when author Paul Monette delivered his brilliant, scathing denouncement of the Catholic Church, then unexpectedly ripped up a portrait of Pope John Paul II. Pope Benedict XVI was just crotchety cruel. But Pope Francis —named for St. Francis of Assisi —had that big smile and genuinely seemed to care about migrants, the vulnerable and the marginalized — like us. He even used the word ‘gay’ instead of ‘homosexual.’
Pope Francis’ reply to a question about a Vatican “gay lobby” on a flight from Rio de Janeiro to Rome made global news. “If a person is gay and seeks God and has good will,” he said in 2013. “Who am I to judge? We shouldn’t marginalize people for this. They must be integrated into society.”
What did this mean? Welcoming inclusion into a family that officially considers us ‘intrinsically disordered?’
And then there was Pope Francis’ interaction with Juan Carlos Cruz — a whistleblower in Chile’s clerical sex abuse scandal.
“He said, ‘Look Juan Carlos, the pope loves you this way. God made you like this and he loves you,'” Cruz told The Associated Press.
Meanwhile the Catholic Church Catechism affirmed, “this inclination, which is objectively disordered, constitutes for most of them a trial.”
Ergo, a behavioral choice.
Therein lies the problem.
LGBTQ people are seen largely as individuals with sinful same sex sexual ‘inclinations.’ So when the pontiff touted ‘the equal dignity of every human being,’ and rebuked Vice President JD Vance with the ‘Good Samaritan’ parable, whereby love “builds a fraternity open to all, without exception” — we are still the exception.
Francis was all also human — having to apologize at one point for using a gay slur. But what of the bigger things like, did he know about the Opus Dei takeover of the U.S. Supreme Court when he chastised Vance about deporting migrants? Did he know that the Archdiocese of Los Angeles agreed to pay $880 million to 1,353 people last October, who allege they were victims of clergy sexual abuse? With a previous payment of $740 million, the total settlement payout will be more than $1.5 billion dollars. Is Leo chipping in to replenish that?
And it’s not over. Earlier this month, Downey Catholic priest Jaime Arriaga, 41, was charged with several counts of child sexual abuse which allegedly happened when he was serving as a transitional deacon at the Our Lady of Perpetual Help Church.
Longtime U.K LGBTQ+ activist Peter Tatchell — who’s campaigned against Catholic homophobia for 58 years — says Pope Francis’ legacy is complicated.
“I extend my condolences to Catholics worldwide on the passing of Pope Francis. While we often disagreed on issues of LGBTQ rights, I acknowledge his more compassionate tone towards sexual minorities. His recent moves to allow blessings for same-sex couples, albeit with limitations, signaled a small but significant shift in Church doctrine,” Tatchell said in a statement.
“However, for millions of LGBT+ people globally, the Catholic Church remains a force for discrimination and suffering. Under his leadership, the Vatican continued to oppose same-sex marriage and trans rights. Catholic bishops lobbied against the decriminalization of homosexuality in many parts of the world. The Vatican still upholds the homophobic edicts of the Catechism, which denounces the sexual expression of same-sex love as a ‘grave depravity’ and ‘intrinsically disordered.’ Francis’s legacy is, therefore, a mixed one — offering some progress, but leaving deep-rooted inequalities largely intact.
“The struggle for LGBT+ equality against a homophobic Church must continue. We urge the next Pope to go further—to end the Church’s support for discrimination, both within the faith and in the wider society.”
Opinions
Gay for pay: Andy Lee and the changing face of content creation
Are the lines between identity and performance more fluid than we’re ready to admit?
In today’s ever-fapping world, the intersection of sexual identity and content creation has become more complicated than ever. Irish content creator Andy Lee, cozily ranking in the top 0% of OnlyFans creators, with his furry physique and tatted up torso, is at the center of the conversation. A self-identifying hetero who rose to prominence during the Pandemic, Lee has amassed a girthy following of horny gays, likely because of the exclusive man-on-man content he has to offer. Yet, his success raises just as many eyebrows as it does trousers. Many question the authenticity of his content, sexual identity and whether or not straight men are overshadowing their openly gay peers.
Claiming to be straight only to then go pole-to-pole on camera, Lee is seen by a significant portion of the queer community to be guilty of queerbaiting (exploiting gay culture for profit). Others can’t help but wonder, is this slab of man-meat genuinely drawn to the physical (and perhaps emotional) experiences he has with men, despite identifying as a thorough(ly) bred breeder?
Lee’s OnlyFans career showcases the blurred, often contradictory nature of sexual identity. He enjoys sexual experiences with men but still identifies as straight, which challenges traditional labels like “gay” and “straight.” His content forces us to confront the nuanced lines of sexual identity, which are rarely ever clear-cut and often defy simple categorization.
The question of authenticity also hangs in the amyl nitrite-scented air. While Lee has said his career on OnlyFans has made him feel “wanted and loved” (and paid) by the gay community, many argue that his identity as a straight man undermines the emotional connection his audience thirsts for. Is his content less authentic due to its “no-homo” viewer discretion warning, or does his openness to explore other men’s bodies reflect the evolving, fluid nature of human sexuality?
This has led to several openly gay performers to claim that, well, “they’re taking our jobs.” They argue that by creating gay content for profit, straight men commodify gay experiences while avoiding the brunt of the stigma that accompanies being openly gay. But how valid is this criticism? In a consumer-driven adult content market, if people choose to engage with Lee’s content, are they unintentionally depriving the gay sex-working community?
And then there is the aspect of the gay gaze (did not stutter). Is it the allure of the forbidden nature of straight men giving into the carnal pleasures that another man has to offer? The taboo? The challenge? Or are they simply the proxy of the coach you had a crush on in high school, the hot trainer who you overheard has a girlfriend, or that college professor you once stood next to at the urinals only to find out for yourself just how extensive his curriculum was? For many, this particular brand of tension is a huge part of the turn-on.
This paradox is just one part of a broader cultural conversation about masculinity and sexual identity. Straight men in gay content can subvert traditional gender roles, while simultaneously reinforcing certain ideals of masculinity. In cases like Lee’s, when a straight man openly enjoys the physical pleasure of being with other men, it speaks to both the complexity and fluidity of sexual identity, and the inability of inflexible labels to accurately and respectfully encompass human desire.
Ultimately, the conversation around gay-for-pay creators like Andy Lee isn’t black and white, straight or gay. Although likely unintentional (let’s be real), these performers challenge existing ideas of identity, authenticity, and the commodification of desire. Whether Lee is queerbaiting, exploring his own sexuality, or just making stacks of cash, his presence in the adult content world invites folks to rethink how we define sexual identity today. Just something to think about next time you’re… enjoying content.
AJ Sloan is a writer, retired adult performer and clinical counseling graduate student. His work has been featured in Huffington Post and The Advocate and led his own weekly column for Fleshbot.
-

 Breaking News5 days ago
Breaking News5 days agoMajor victory for LGBTQ funding in LA County
-

 Features5 days ago
Features5 days agoKoaty & Sumner: Finding love in the adult industry
-

 Commentary3 days ago
Commentary3 days agoBreaking the mental health mold with Ketamine: insights from creator of Better U
-
 Miscellaneous4 days ago
Miscellaneous4 days agoCan you really find true love in LA? Insights from a queer matchmaker
-
 Arts & Entertainment4 days ago
Arts & Entertainment4 days agoIntuitive Shana gives us her hot take for July’s tarot reading
-

 Movies1 day ago
Movies1 day agoTwo new documentaries highlight trans history




