Commentary
A Half-Baked Ruling
A cake is not speech

 On February 5th, Kern County Superior Court Judge David R. Lampe issued a ruling denying the California Fair Employment and Housing Commission’s request for a preliminary injunction that would have ordered a baker to stop discriminating against same-sex couples, pending trial in a case.
On February 5th, Kern County Superior Court Judge David R. Lampe issued a ruling denying the California Fair Employment and Housing Commission’s request for a preliminary injunction that would have ordered a baker to stop discriminating against same-sex couples, pending trial in a case.
The case arose after Eileen and Mireya Rodriguez-Del Rio visited Tastries, a commercial bakery in Bakersfield, and selected a cake design for their upcoming wedding reception based on one on display in the shop. According to Judge Lampe’s decision, the couple did not request any words or messages on the cake. When they returned for a tasting a week later, the store’s owner, Cathy Miller, told them—apparently based on her religious views—that she does not condone marriages of same-sex couples and they therefore would have to go elsewhere for their cake.
Faced with the indignity of being shunned and told “we don’t serve your kind,” the couple filed a complaint with the agency that enforces California’s law barring sexual orientation discrimination by businesses. The agency agreed that that law had been violated and sought the order Judge Lampe denied.
The judge did not reach whether Ms. Miller had a religious freedom right to deny the couple equal treatment. Instead, his decision was based on free speech grounds. He concluded that, “The State cannot succeed on the facts presented as matter of law” because, in his view, “The right to freedom of speech under the First Amendment outweighs the State’s interest in ensuring a freely accessible marketplace.”
Either now or after Judge Lampe grants the motion to dismiss the case Ms. Miller’s lawyers have said they will file, the government agency likely will appeal.
Judge Lampe’s ruling is wrong and dangerous, and hopefully an appellate court swiftly will overturn it. Every other U.S. court to have considered similar First Amendment claims advanced by bakers, florists, photographers, invitation designers, and reception halls has rejected the arguments on which Judge Lampe relied.
Lower courts did that in a very similar case, known as Masterpiece Cakeshop, Ltd. v. Colorado Human Rights Commission. That case was argued to the U.S. Supreme Court December 5th. A decision should be released by the end of June. If the justices follow past rulings, they too should refuse to license such discriminatory acts.
While there is an absolute right to believe what one wants, and a near absolute right to say what one wants (subject to laws regulating defamation, invasion of privacy, harassment, threats, and similar wrongs), the U.S. Supreme Court has rejected any First Amendment right to engage in discriminatory conduct. Discriminatory treatment is conduct, not speech.
Judge Lampe analogized the situation before him to cases involving compelled speech. Those cases hold that the government can’t force students to salute the flag, can’t compel individuals to display a state motto they object to on their vehicle license plates, and can’t require newspapers to publish the replies of political candidates whom they criticized. There are at least three problems with that comparison, however.
First, the state agency here wasn’t seeking an order that Ms. Miller say anything. A cake is not speech. And, to the extent a wedding cake conveys a message of some sort, it’s the message of the betrothed couple who chose the design, not the baker they asked to follow their instructions. But, beyond that, all the state agency sought was an order that Ms. Miller not discriminate by refusing to make cakes for same-sex couples she makes for everyone else. If she couldn’t abide the thought of a custom wedding cake she made being enjoyed by those at same-sex couple’s receptions, she could just stop making such cakes altogether
As raised during the Masterpiece Cakeshop argument, it also would be difficult to draw a line between Ms. Miller and others who believe some people aren’t worthy of equal treatment. If a wedding cake is constitutionally-protected speech, what about the catered wedding meal, floral arrangements, hairstyles, and make-up applications? It likewise would be hard to limit a ruling to weddings. And, if people have a conscience right not to treat same-sex couples equally to others, why should they have to provide equal service to those of particular races, nationalities, or religions? If the Constitution meant that, minorities once again could be legally treated like pariahs in this country.
When Judge Lampe valued a business person’s “freedom of conscience” over customers’ equality, he erred. The notion that one is complicit in how others use what one creates wrongly imposes one’s beliefs on others. Most importantly, people who go into commerce—even commerce involving expression—properly are subject to the rules governing all businesses. Those selling their paintings can’t use toxic materials or plagiarize, even if their beliefs dictate it. Even with art, neither religion nor speech should be trump cards.
Jon W. Davidson has been a leading LGBT legal rights advocate and constitutional scholar for more than 30 years. He recently stepped down as the national legal director of Lambda Legal.
Commentary
When optics matter more than harm: BAFTA, BBC, and editing solidarity while letting slurs slide on through
A polite examination of where priorities lie when the BBC chooses to censor political solidarity yet allows a racial slur to air unedited, and what this might say about the industry as a whole

The night was meant to be a celebration. At the British Academy Film Awards, an institution that claims to pride itself on honoring the best in international cinema, the cast and creatives of Sinners arrived as nominees, as artists, as guests. Instead, they were confronted with a word that should have no oxygen left in public life.
On stage, actors Michael B. Jordan and Delroy Lindo were visibly jarred. You could see it flicker across their faces, the moment when shock and dismay meet recognition. And yet they both proceeded unflinchingly with grace and poise, because that is what Black people so often have to do to keep progress progressing. Tough skin. Resilience. Smile through it. Keep it moving.
But what is undeniable is the weight. The weight that that particular slur carries, especially when it comes from the mouth of a white person. It carries centuries of hate, atrocities, and trauma. It echoes lynchings and segregation, caricatures and exclusion. It is one of the most violent linguistic relics in the English language, and it is an undeniable trigger, a generational trauma that continues to afflict an entire demographic of the population. There is no casual context in which it lands softly, and no stage vast or shiny enough to dilute its history.
BAFTA eventually apologized. Too little, too late. This is your stage, and these are your guests. It is your responsibility to protect and advocate for them in the moment, not hours later when headlines begin to circulate. Award shows have removed attendees for far less. If a guest shouts a bomb threat, if someone storms the stage, or if there is a physical altercation, swift action follows. Why, then, does a quintessentially racist slur prompt hesitation? Why is decorum preserved more urgently than dignity?
Complicity is far too telling, and passivity is far too common. When celebs like Neil Patrick Harris retreat behind tiresome labels of “apolitical,” what they are really aiming to guard is not neutrality but comfort. As a gay white man, Harris exists in a space where his privileged identity eclipses his marginalized identity. His queerness can be selectively foregrounded, while the protections afforded by his whiteness shield him from realities faced by communities who wear their otherness on their skin. This insulation Harris possesses makes silence that much more palatable to his tongue.
Hollywood no doubt understands the power of narrative control better than any industry. Edward Bernays, the nephew of Sigmund “Uncle Sigi” Freud, built the blueprint for modern propaganda by teaching institutions how to shape perception, manufacture consent, and quell public outrage. That legacy of image management continues today with folks like with Netflix co-founder Marc Randolph, Edward Bernays’s own nephew (runs in the family). The industry knows how to redirect attention, isolate incidents, and reframe harm as a simple and easily forgivable and forgettable misunderstanding.
Back to the BAFTAs, I understand that John Donovan lives with Tourette’s syndrome, and that tics are involuntary. This reality deserves full acknowledgment. Neurological conditions are not punchlines, nor are they moral failings. But accountability and accommodation can coexist. One question remains conspicuously unanswered in much of the coverage: did Mr. Donovan, as “mortified” as he claims to have been, immediately excuse himself from the room? Did he remove himself from the space as soon as the word left his mouth? Or were his apologies as delayed as BAFTA’s?
Too many are quick to reduce the entire incident to a diagnosis, as though that ends the conversation. If this grown man is of sound mind enough to create and promote a film about his experience living with Tourette syndrome, then surely he is also capable of understanding the magnitude of that word and the necessity of immediate harm mitigation. A condition may explain behavior. It does not erase impact. It does not absolve institutions from responding decisively.
Coverage has framed the moment as an isolated incident during the awards ceremony. But Sinners production designer Hannah Beachler tells a different story. “I keep trying to write about what happened at the BAFTAs, and I can’t find the words. The situation is almost impossible, but it happened three times that night, and one of the three times was directed at myself on the way to dinner after the show.”
Three times.
Why, then, is most coverage focusing solely on the on-stage incident? Because that one was caught live, in front of cameras, in front of an auditorium of witnesses. It is easier to contain a scandal to a single viral clip than to interrogate a broader culture. But if it happened three times in one evening, the problem is an environment, not a single tic-induced outburst. Again, BAFTA, who are you letting into the party? What safeguards are in place? What standards are enforced when the cameras are off, and the ancillary festivities and dinners begin?
One glaring example of misplaced priorities came when the BBC chose to edit out filmmaker Akinola Davies Jr’s call to “free Palestine” from its televised BAFTA coverage, while simultaneously failing to remove the audible racial slurs. Folks couldn’t help but take notice that both decisions happened within the same two-hour tape-delayed broadcast window, yet the network found time to censor a politically charged solidarity statement while allowing the slur to slide through unscathed. This discrepancy raises questions about what content editors deem unacceptable versus what they allow to reach millions of viewers. The caucacity is truly mind-boggling and blood-curdling.
The fact that this occurred on such a prestigious platform in 2026 and was met with delayed apologies that skirt clear culpability is precisely why Black history cannot remain a neatly packaged 28-day-long pat on the back. It must be in the curriculum in schools. It must be contextual in conversations. It must be uncomfortable because it is necessary. Because when people understand the lineage of that word, its architecture of harm, its function as a weapon, maybe, just maybe, they will treat it as such.
This isn’t about political correctness. It is a matter of institutional responsibility and whether global stages will continue to rely on the grace of Black artists to absorb humiliation in real time. Progress does not sustain itself on resilience alone. It requires intervention and accountability. And sometimes, it requires cleaning house before you roll out the red carpet again. Michael B. Jordan and Delroy Lindo, you two kings have stoicism and poise that far surpass my own. That said – Take a seat, BAFTA, you arcane fraternity of troglodytes.
Commentary
Post-Valentine’s Day: Are your standards protecting you — or keeping you single?
As a matchmaker working with LGBTQ folks across the country, I see one pattern over and over again: we are dating with clipboards.
Valentine’s Day has a funny way of magnifying things.
Maybe you promised yourself this would be the year you’d really try: more dates, more effort, more vulnerability. Maybe you did. Maybe you went on five, ten, or fifteen dates. Maybe you tried so hard you’re exhausted.
And yet… here you are. Still single.
Or maybe you’re sitting with a different regret, that you didn’t put yourself out there enough. That you swiped half-heartedly. That you canceled that second date because something felt “off.” That you let another potential connection slip through your fingers.
As a matchmaker working with LGBTQ folks across the country, I see one pattern over and over again: we are dating with clipboards.
We treat dates like job interviews.
We’re evaluating resumes.
We’re checking boxes.
Does he make enough money?
Is he educated?
Does he travel?
Is he top, bottom, or vers?
Is he emotionally available?
Does he want marriage? Kids? A house?
Is he tall enough? Attractive enough? Ambitious enough?
And if he checks every box? Great we’ll proceed.
But what if the real connection isn’t on the checklist?
The Checkbox Trap
Somewhere along the way, many of us decided that compatibility means alignment in every category. We want someone who mirrors our hobbies, our career trajectory, our lifestyle, and even our sexual preferences permanently.
But here’s what I hear constantly from clients:
“I was a top for years. Then I was vers. Then I preferred bottoming.”
“We opened things up later.”
“My priorities changed.”
We evolve. Our sexuality evolves. Our careers evolve. Our emotional needs evolve.
Yet we treat these things as fixed deal breakers before we’ve even allowed chemistry to breathe.
Sexual compatibility matters. Emotional availability matters. Shared values matter.
But are we confusing preferences with prerequisites?
How Many Deal Breakers Do You Need?
By the time many men reach their late 30s, 40s, or 50s, the list has grown long. Very long.
No actors.
No entertainment industry.
No one who earns less.
No one who earns more.
Must want monogamy forever.
Must want children.
Must not want children.
Must be “settled.”
Must be “ambitious.”
Must be hot.
And then we wonder why we’re still single.
I’m not saying abandon standards. I’m asking: are your standards protecting you from incompatibility or protecting you from vulnerability?
Sometimes the truth is harder. Sometimes we seek a partner who feels “worthy” enough so we can feel worthy by association. If I’m with someone impressive, then I must be impressive. If I’m with someone accomplished, then I must be accomplished.
But real intimacy requires something else entirely: self-worth.
When you feel worthy within yourself, you don’t need your partner to prove it for you.
The Twin Flame Mirror
There’s a concept people love to talk about: twin flames.
Whether or not you believe in the term, the idea is powerful. A person who mirrors you. Reflects your strengths and your flaws. Someone who activates you deeply.
What most people don’t realize is that mirrors aren’t always comfortable.
That person who feels “too emotional,” “too guarded,” “too intense,” sometimes they are reflecting parts of you that you’ve worked hard to avoid.
The chemistry may be electric. The connection may take time to unfold. But if you dismiss someone after one date because they showed a crack in their armor, you might be rejecting a growth opportunity.
One date is rarely enough.
People are nervous. Guarded. Performing. It often takes two or three dates before someone relaxes into who they really are.
Attraction vs. Alignment
Yes, you should feel attraction.
But attraction grows.
I’ve watched clients pass on kind, emotionally available, stable men because the spark wasn’t immediate, only to later chase someone wildly charismatic and completely unavailable.
The butterflies you crave? Sometimes they’re anxiety.
The quiet steadiness you overlook? Sometimes that’s security.
If you want the life of the party, ask yourself: are you willing to walk into the party and introduce yourself? Or do you actually need someone slightly more grounded? Maybe an ambivert instead of an extrovert. Maybe someone who lights up in intimate settings rather than on stage.
Compatibility isn’t about sameness. It’s about complementary energy.
Letting Go
After Valentine’s Day, a lot of men insist they’re fine being single. And yes, you can have a full, beautiful life alone.
But let’s be honest. Holidays can sting.
That quiet moment when everyone else seems partnered up. That subtle ache. It’s real.
So instead of doubling down on stricter standards this year, what if you softened?
Letting go. Letting go. Letting go.
What if you stopped asking, “Why won’t this work?” and started asking, “Why could this work?”
What if you looked for green flags instead of scanning for red ones?
Rethinking Monogamy (Without Throwing It Away)
Let’s talk about the word that sends everyone into debate: monogamy.
I believe in monogamy. I’ve seen it thrive. I’ve seen beautiful long-term partnerships built on it.
But monogamy is not declared- it’s developed.
It’s built. It’s earned. It grows from connection.
You don’t have to decide on the first or second date that you’re committing to sexual exclusivity for the rest of your life. And you don’t have to dismiss someone because they’re open to a conversation about what commitment might look like over time.
I’m not saying abandon your values.
I’m saying don’t brush someone off because their view of relationships isn’t identical to yours on day one.
Connection leads. Structure follows.
So Here’s the Question
How many more people do you need to cycle through before you allow one to stay?
How many more perfectly “qualified” bachelors do you need to interview before you realize you’re searching for a feeling, not a résumé?
This year, try something radical:
Give the second date.
Give the third.
Let attraction build.
Let flaws exist.
Let yourself be imperfect too.
Because the goal isn’t to find someone who checks every box.
The goal is to find someone who makes you smile in the middle of a sentence for no reason at all.
And if you can feel that?
That’s not on a checklist.
That’s connection.
If you are ready for a connection join my gaytabase and let’s see who I can connect you with-
Join the Los Angeles Blade, Daniel Cooley, and AJ Socal for our second, free, gay singles mixer at the Abbey this Thursday at 7 pm. It is a low-key and fun way to meet other singles.
Daniel Cooley is a gay matchmaker & co-owner of Best Man Matchmaking – California’s premier service for queer and trans men seeking emotional connections. Learn more here.
Viewpoint
Gay acceptance in US takes a dangerous reversal
Last five years should be wake up call for movement

Shocking news has arrived. New social research says it’s true. Gay, lesbian, gender fluid people, and their allies: we have a problem.
New bias attitude research published by respected social scientists Tessa E.S. Charlesworth and Eli J. Finkel of Northwestern University, based on a longitudinal research program, has shown that gay acceptance in the U.S., which reached its peak about 2020, has taken a deep nosedive in the opposite direction during the last five years. The researchers exclaimed, “This reversal stunned us” — as it did me.
What makes this reversal even more remarkable, as the two social scientists explained, “Americans’ bias against gay people declined faster than any other bias ever tracked in social surveys.” It appears that a new cycle of hetero supremacy has arrived. More likely, the hetero supremacists never went away — just stewing revengefully out of sight around the corner with their buddies from white supremacy and male supremacy.
Analysis of 2.5 million American responses from the beginning of 2021 through 2024 revealed that progress had been turned around. In just four years, anti-gay bias had risen by 10 percent. Researchers followed both explicit bias (to what extent do you prefer straight people over gay people?) and implicit bias (more automatic responses inferred by how rapidly people associate words, such as straight with “good” and gay with “bad.”)
Most disturbing of all, these trends were particularly strong among the youngest American demographic, those under 25, a society’s hopes for the future. Also noteworthy was that anti-gay bias has grown faster among conservatives, but it had also risen among liberals.
The researchers admit they have no idea what is causing this dramatic reversal. They suggest two possible hypotheses: (1) anti-trans bias and (2) fear of gays grooming children to become gay, an essential part of hetero supremacists’ baggage of hate for the past 125 years in the West. Children cannot be groomed into being gay but are born that way for an evolutionary reason (more on that subject in a later article.)
Let me add a third hypothesis based on my close, active involvement and observation as a gay community organizer over the past 60 years. A big part of the problem is gay people themselves. If you have followed my many writings over the past 25 years, you have heard this sermon several times before in varying language and contexts.
The Gay Liberation Revolution (1969-c.1985) taught gay and lesbian people that gay peoples’ self-acceptance and united action are more powerful than hetero supremacy. A Gay Liberation tidal wave provided the momentum for a “movement” forward for our people. Now, that tsunami has become a ripple. How did that happen?
1. The absence of a gay political movement. A political movement is “an organized effort to promote or obtain an end.” There are people who I respect who delusionally speak as if a gay movement still existed. A Gay Liberation template does exist for what a gay movement might look like. It must be played forward, however, with the language, reality and tools of today. It begins with the question: How am I and my community oppressed today by hetero supremacy? Action grows out of oppression.
2. The dominant ideology of gay assimilation. As James Baldwin preached, assimilation is always done on the terms of the dominant culture. For gay people, assimilation implies the eradication of hard-fought-for community and identity. Gay and lesbian people, where did you disappear to? Just yesterday, you were here with your fists in the air.
3. Elite capture of the gay community. This capture is characterized by a top-down power structure (elite vertical axis), community members (grassroots horizontal axis) becoming passive spectators, and the primary priorities being wealth, donors, and celebrities, not community well-being. The call for gay power devolved into donate and consume.
4. Community fragmentation by visual media. The dark side of the current new tech visual media avalanche is the fragmentation of a formerly good-enough-united gay community. Visual media has turned community awareness from “we” to “me.” Local news and investigative journalism have disappeared completely from gay news sites that are now “curated.” A good example was the implosion of Outfest: the LGBTQ Film Festival in L.A., a major community cultural institution for half a century. Gay people found out about that truly shocking community news after Outfest’s disappearance by an investigative journalist at the Hollywood Reporter;the financial malfeasance of GLAAD was uncovered by the New York Times, not gay news sites. Without investigative journalism, community members do not have the information spotlight that is essential for being actively involved and engaged in a healthy community.
5. Pick off the low hanging fruit first. I often hear from others that trans people have taken over the movement. My standard reply: “Because gay and lesbian people have voluntarily disappeared from their political movement, a vacuum has occurred. Vacuums are always filled by something. Trans people are not the problem. There is a problem: your disappearance. The main problem, however, and never forget this, is hetero supremacy.” The hetero supremacists’ playbook is the same used to rescind Roe. Get the low hanging fruit first — under 18 trans youth. Then, proceed calculated step-by-step to the main target — YOU AND ME. Supreme Court Justices Alito and Thomas maladroitly revealed their goals: (1) rescind gay marriage and (2) recriminalize same-sex sexual acts.
A dark night of the gay community’s body and soul might be coalescing. As with all such dark nights, a new sun will rise with renewed vigor and vision, with gay righteous mind and mindfulness replacing today’s mindless scrolling, streaming and surrendering. As the old United Negro College Fund wisely said, “A mind is a terrible thing to waste.”
Don Kilhefner, Ph.D., is a pioneer gay liberationist and a gay community organizer in Los Angeles, nationally and internationally for the past 60 years.
Commentary
Valentine’s Day, Alone
We the People are embracing and uplifting our own and each other’s humanity.

Valentine’s Day. Permission to briefly set aside mental acrobatics and just feel. Over the years, I’ve gone from Elvis’ “Can’t Help Falling in Love” to the lesbian version of Beyonce’s “Single Ladies.” And after we won marriage equality, I shed happy tears to “Same Love” by Macklemore & Ryan Lewis and Mary Lambert, even though I was alone.
The truth is, my longest relationship lasted five years. I don’t need therapy to tell me it’s my fault. I always secretly hoped that each woman would rekindle the flames of my first love. Yes, she was straight, and it was incredibly complicated – but it was also the Age of Aquarius, and for this budding Aquarian hippy-wannabe, it was mythologically perfect, as doomed as I subconsciously knew it was.
So, Valentine’s Day always had a slight shade of pain.
But I had my dogs. I didn’t need romance – I needed love. And over the years, what happy times we had, watching some action movie and sharing the crust of a great Hawaiian pizza.

I thought this Valentine’s Day would be the same. Actually, Pepper, my 18-year-old Cairn Terrier, has been my longest relationship of all. I rescued her when she was five. She was living in a Latino family, beloved by a young teenage boy who called her Sparky. But one of their two other dogs didn’t like her, so they had to give her up for her own safety.
The boy tried so hard not to cry when they dropped her off – but Sparky wailed and wailed. My neighbors looked out to see what was wrong. I did what I could to ease her sense of abandonment. I even learned a little Spanish and changed her name so she wouldn’t be retraumatized every time I called for her. My other poodle-ish dog, Charlie, and I had to wait for her to trust us.
In time, Pepper and Charlie bonded. When he got sick, I took her to hang out with him in the hospital, bringing her home at night. Charlie died of a seizure overnight without us.
Not long after, my friend Gloria Nieto called to see if I would be interested in adopting this little boy dog who needed a new home asap. Gloria lived in the Santa Cruz area, so we decided to meet halfway in San Luis Obispo to see if the two dogs got along. They did, Papa D came home with us, and I became friends with Papa D’s heartbroken mom on Facebook.

Pepper and renamed DeeJ bonded quickly, with Pepper becoming something of a mother. One time, I was surreptitiously watching them play at a wonderful doggie day care on Ventura Boulevard. The attendant wasn’t in the room when a bigger dog started menacing DeeJ, who backed into a corner, shaking. Pepper went and sat next to DeeJ, but when the bigger dog didn’t back off, Pepper, who was also scared, got on her belly like a supplicant and crawled between the bigger dog and DeeJ. I ran back inside to get them and take them home to West Hollywood.
I’ve never forgotten Pepper’s incredible bravery, inspired by love. When DeeJ died, we were both bereft. At times, we would independently hear a sound like a bowl being moved in the kitchen and look up, expecting DeeJ to come out and bound across the floor at any moment. Then we’d hug.
After a while, I adopted Keely, who was deaf. Keely wasn’t interested in bonding with Pepper. But she wasn’t with us very long – she had a massive cancerous tumor, and the prognosis for survival after surgery wasn’t good with her other ailments.
After Keely died, I decided Pepper would be the only dog. The two of us, alone. And despite having Cushings, having to undergo surgery for a small tumor, developing kidney disease, and starting the beginning stages of doggie dementia, Pepper was doing incredibly well.

And she was incredibly sensitive to my moods. On Wednesday, Feb. 11, after we’d come home from her grooming, I tuned into ice dancing at the Olympics. The Canadian couple skated so beautifully to “Starry, Starry Night,” tears started streaming down my face. Pepper bolted up, looking at me quizzically but with doggie empathy before coming over to lick my tears and give me kisses. She eased slowly across my chest to hug me.
The song stuck with me, looking at the waning crescent moon as we went on our brief nightly walk. In the carport before we came home, we ran into our neighbor and her young Shih Tzu from the building next door when another neighbor and his big dog came down the alley. Suddenly – in a flash – the big dog jumped up, tearing off his leash, and lunged towards the Shih Tzu. Seconds later, she jumped onto Pepper.
We all freaked. I was knocked down in the struggle to free Pepper. By the time I got to her, she was listless and bleeding – but still had a pulse. Another neighbor madly dashed us to the Emergency vet as I told Pepper how much I loved her and to please stay with me. But she couldn’t. She died in my arms.
I was devastated but not freaked out – I’ve held dying friends and dying dog/kids before. But the sudden violence I was powerless to prevent made this different. My apartment was suddenly big and empty and quiet – even with TV politics in the background. Images of Pepper’s bloody body lying on the concrete blinded me. I blurted out her name and reached for where just hours earlier she snored softly, her skinny, aging body snuggling next to mine. I changed channels, looking for something comfortably mind-numbing. Unbelievably, I came upon a replay of the Olympics and “Starry, Starry Night.”
After a sleepless night, I had a 12 Step phone call with a friend who lost her precious cat last May. She suggested that this first stage of denial was akin to the deep, difficult First Step of surrendering. That made sense to my journalist/observer side, who advised my jumbled emotional side to be patient and, as 12 Steppers say, “feel the feelings” when they come.
This June, I’ll be 46 years clean and sober. But I now feel like a newcomer again. That’s good because it gives me permission to be weak, to acknowledge that I need help, and accept the love that’s being so generously offered.
And here’s where this tragedy becomes extraordinary.
Early next morning, my 12 Step neighbor – who’s 88, BTW! – knocked on my door. She brought a bag of food from someone from the building next door, who was among the slew of neighbors who rushed out, hearing our anguished cries. She said it felt like community – even though we only knew each other through our dogs. I was Pepper’s mom.

And this made me hesitant to report what happened. As I struggled to get up and get to Pepper, I saw the father of this big dog hold him tightly and break down. “I can’t lose another one,” he cried over and over to his wife. Apparently, he just lost his father. We all didn’t need a second tragedy. But Pepper’s death was a preventable fatal accident, and he still had to be accountable.
I struggled with this. Knowing him as a dog-loving neighbor, I suspected he and his family were devastated. So, I forgave him and the big dog, who was so sweet on the street. I then called several neighbors, thanking them and asking for advice. One neighbor felt it was important to report because this dog had bitten two other dogs over the years, and what if this dog attacked a person? Another neighbor understood my dilemma and offered to back me up, no matter what, but said she no longer felt safe in the community.
And there it was. Yes, my feelings mattered – probably tied to my guilt at not being able to protect Pepper, as this man was trying to protect his dog/child from certain execution. But community mattered more.
Then the big dog’s mother called, totally devastated and deeply apologetic. They have two young daughters whom they’re trying to teach about doing “the right thing,” so they had already called Animal Control to report what happened and find out what to do next. I told her that I forgave them – but they had to be mindful of community safety. I also asked her to please teach their children that not every bad event demands rage and retaliation in response. Love and understanding are really important right now.
She cried and called back later to say they had decided to put their beloved big dog down themselves so they could say goodbye as a family. Our community has responded with empathy and support for them now, too.
So, while I continue to struggle with feeling my feelings and realize that this Valentine’s Day, I really am alone, I also feel surrounded by love, including from my MAGA friends, and thinking of DeeJ and Pepper reunited.

There is something going on. Not just here, in our little corner of West Hollywood embracing tragedy and forgiveness; or in anti-ICE protests remembering Renee Good and Alex Pretti; or the almost universal outpouring of love and joy in Bad Bunny’s Super Bowl halftime concert.
We the People are embracing and uplifting our own and each other’s humanity.
Sing it with me: “What the world needs now is love, sweet love. It’s the only thing that there’s just too little of.”
Happy new post-Valentine’s Day!
This essay is updated/cross-posted from longtime LGBTQ+ journalist Karen Ocamb’s Substack LGBTQ+ Freedom Fighters.
Commentary
What Grindr’s pricey new subscription says about the gays, intimacy, and capitalism in the age of AI
Grindr’s shiny new Edge subscription epitomizes how dating and hook-up apps monetize loneliness by selling algorithmic control as a substitute for genuine human connection

This February, Grindr discreetly started testing out a brand new premium subscription tier, Edge (props on the wordplay), powered by its proprietary generative AI stack appropriately named “gAI™.” The catch is that some users are being asked to pay more or less the price of one hour of an escort’s time for one month’s subscription. This would place Grindr’s top tier soaring above most mainstream dating apps (Tinder, Hinge, Bumble, etc.) with prices higher than Nicki Minaj on a MAGA stage, some can’t help but wonder who the target consumer is.
At face(less) value, this feels like a corporate strategy to squeeze more money out of a perhaps struggling “dating” app. Grindr’s stock has gone limp, and it’s pushing AI as the ED med that will fluff it up into a smarter, faster, more personalized user experience. But when you really look at it, this pricing experiment speaks volumes about the current state of our gay community, intimacy, desire, and the toxic top that is capitalism in the age of artificial intelligence.
Grindr entered the scene (and the app store) in 2009 as a simple and sweet grid of nearby dudes scoping out who’s around and down to get down. It was immediate. It was raw. And, perhaps most uniquely, it was physically grounded. But like most apps and platforms do over time, features were paywalled, and basic functions became privileges. The free portion of the grid shriveled like a pair in winter air. Ads multiplied and became more aggressive, like a digital strain of super gonorrhea. Want more? Pay. Want to be seen? Pay. The death grip of capitalism knows no lube.
This transformation is a testament to a larger pattern in tech called enshittification (aka crapification), where platforms become increasingly more hostile to their users as their money-goggles fog up with greed. Grindr’s Edge is the latest example; a subscription promising personalized AI-generated matches and chat insights, all with the promise of more “meaningful connections.” With price hikes reaching close to half a grand, one can’t help but wonder what is actually being commodified here.
Gay lust is no stranger to consumer culture. From marketing fitness (“Look Better Naked”) to gay-centric grooming (shoutout to Good Head, we see you king), sex drive and commerce have been bedfellows longer than the grandparents from Willy Wonka. Hook-up and dating apps, simply put, commodify attention. Profiles are products. Swipes are currency. Desirability is now quantifiable, folks. Take this concept, feed it one too many bumps, and you’ve got Edge.
What’s happening, my fellow homosexuals, is the premiumization of intimacy. Not just matchmaking, but the promise that technology can deliver connection… for the right price. And the price of this new tier of service says more about our collective culture at this moment than it does about the greedy little piggies behind Grindr. We live in an age where AI is infringing on emotional territory once thought to be uniquely human. Algorithms already curate our newsfeeds, recommendations, and shopping lists. And now, well, we can tag “digitally omnipotent yenta” to the tally.
The creation of Edge also highlights how modern capitalism treats desire as an inefficiency that can be solved. Grindr is utilizing a not-so-new strategy here: hone in on its users’ loneliness and fear of rejection and redesign features that address these feelings… at a premium. One undeniable takeaway is that genuine interactions are no longer occurring naturally.
On a psychological level, Grindr’s Edge subscription tugs at the arguably universal hunger for control. In a world brimming with flirtations that flatline, DMs that die down, and dates that don’t pan out, the allure of AI as a fail-safe is, well, seductive. But what happens when that illusion of control clashes with the actual intimacy that we seek? Instead of enhancing connection, AI could fossilize it, making real human interactions that much more transactional than said apps have already made them out to be.
Grindr’s Edge experiment reveals how capitalism monetizes the desire for human connection, how tech sells the guarantee of ease void of authenticity, and how intimacy in the digital age increasingly becomes a slave to the algorithm. Yet resistance is already clapping back. Online discourse from users dragging Grindr for the high prices and migrating to alternative platforms shows us that many are not buying into the premiumized dream.
Ultimately, Edge feels less like an innovation and more like an admission: that instead of fostering environments where vulnerability and spontaneity thrive, platforms would rather engineer a shortcut and charge stratified admission. When the illusion of confidence is packaged as a purchasable upgrade, the entire thing starts to feel that much more bleak. Stripped of its shiny branding, it reeks of incel-scented desperation, a tech-mediated fantasy that mistakes control for chemistry and convenience for closeness.
I may stand alone in this humble opinion, but a dude who’s audacious (or foolish) enough to sign up for such a service is a hard pass. In the end, shop local – hire an escort. At least then nobody is denying the pure transaction of it all.
Commentary
Are we done with ‘Drag Race?’
While the show may feel a bit formulaic, and we long for the days of earlier seasons, where we met luminaries like Alaska, Jinkx Monsoon, and Bob the Drag Queen, the larger question is whether the show is more focused on straight audiences.

RuPaul’s Drag Race has left an indelible mark on history. What started as the bastard love child of America’s Next Top Model, Real Housewives, and Project Runway has birthed an entire industry of drag race content, from tours to review podcasts. It’s elevated its stars to international stardom and reshaped the queer economy with its impact on bar culture, marketing to queer people, and Mama Ru pushing her girls to sell.
While conservatives have declared war on drag, the show has held strong. Now in its latest and 18th season, a show that has united the whole LGBTQ community in inside jokes and pop culture references has offered the community its own sports equivalent and instant “in” to a conversation.
The question arises: Are we done with Drag Race?
Considering how Heated Rivalry became a ratings behemoth despite being an independent Canadian drama, and viewers seem more galvanized about the queer representation on The Traitors, have we developed Drag Race fatigue? The show hit a high point with franchises in countless countries, with RuPaul even crossing the pond for the UK and the earlier versions of the Australian series. The political and economic fuckery of our current state of affairs has even hit Drag Race.
While the show may feel a bit formulaic and we long for the days of earlier seasons, where we met luminaries like Alaska, Jinkx Monsoon, and Bob the Drag Queen, the larger question is whether the show is more focused on straight audiences. In a post-Trixie & Katya world, it seems there’s a choice in the world of drag: are you courting queer or cis-het audiences? Do you become gay famous and never pay for a drink again, or do you pander to straight women and make bank?
The issue may not be that Drag Race as a show has become the problem, but it’s just become too normative. How could a show with new queens each year feel…less than fresh?
The show seems to have drawn a line in the sand by defining what is “good drag,” so you end up with a cast that could be anyone with a Sephora gift card, OCD, and a budget for lavish costumes. The latest season broke from its recent trend of casting young, social media-savvy queens opting for more seasoned performers in their 30s and 40s. They’re then labeled as old. “Be still, my heart!”
Part of what drove the show and the major cultural movements was queens being themselves and finding artistic solutions to their shortcomings. But we’ve reached ouroboros with queens communicating entirely in Drag Race references. The contestants are self-producing and trying to force storylines, catchphrases to sell merch, and court a yet-to-be-determined audience to try to make back the money they invested or try to stay relevant in a pool of girls that’s reached three digits.
The show is becoming a bit too self-aware. The challenges are a bit repetitive, and seasons of Drag Race are starting to feel a bit like a Law & Order episode. By episode 4 or 5, you can peg who is the winner, who is the delusional starlet whose ego RuPaul must crush to claim 7 more years of youth (hi, Jan!), and who is the villain.
The predictability betrays what’s behind the curtain. There’s a bit of manipulation to venerate queens who have the savvy to carry the brand. But is it at the cost of some of the show’s integrity? For example, this season, it was clear Mandy Mango was not on par with the other girls with regard to styling and make-up, but having the judges tell us that she wasn’t funny in her sketch or that she didn’t win a lip sync feels a bit too far. In an era of “fake news” and media manipulation, can you trust a show that tries to tell you the sky is not blue but fierce?
In an earlier season, a personality like Mandy’s might have won, a la Jinkx Monsoon. There is also all that we don’t see, given a notoriously toxic fandom, the show runs the risk of activating a fanbase primed with racist torches and pitchforks.
It’s an open secret that RuPaul’s Drag Race is more of a reality show than a competition, but that might be impacting its longevity. With Tyra Banks facing a documentary covering some of her insane stunts on America’s Next Top Model while Project Runway is still alive and kicking, it’s clear that if Drag Race wants longevity, it needs to value its integrity.
After all, in an alternate timeline where Drag Race was honoring its LogoTV roots, it might have featured Connor Storrie and Hudson Williams as guest judges or tapped Alexander Skarsgard from Pillion rather than female celebrities who offer the A or B-list equivalent of bachelorettes at drag brunch like the now-canceled Nikki Minaj and Whitney Cummings.
As we careen closer to an autocracy, do we deserve a reality show that keeps it real? We have reached a point where what we have allowed to continue has come to bite us. Choosing capitalism over integrity is a tacit support for corruption. In a time where the queer experience is fundamentally unfair, should we have a reality comparison that’s inherently unfair?
All this being said, Drag Race is still doing its part to support the bar industry. Some viewers have found it hard to watch Drag Race without purchasing episodes, potentially because its ties to CBS/Paramount/MTV World of Wonder are still creating content for the community.
Canada’s Drag Race still takes chances and casts a diverse group of queens, and it seems like a fairer contest. Surviving a revolving door of hosts, the show has managed to stay fresh and engaging. Drag Race UK also has retained a lot of the interqueen chemistry that drives the show with drag queens who know how to read, kiki, and maintain good working relationships rather than pandering to television drama.
Drag Race is essentially sports for people who don’t like sports. Drag Race gives us our own arena where our queers can highlight aesthetics, drama, stunts, and humor. We all make our draft picks during the Meet the Queens premiere, and we wear merch for our favorite players. But if the show divests from queer culture to make a buck, you end up with straight women criticizing the work of multiple artists and tens of thousands of dollars of effort because they don’t like someone’s aesthetics or they have “bad make-up.”
The show started as a platform for a forgotten but timeless art of queer people dressing up as women to lampoon toxic masculinity and internalized homophobia while serving as den mothers, brassy broads, and queens of our community to help make being gay a little more fun, flirty, and cunty.
I hold out hope for Drag Race, but I do think it would serve them to be a bit more beholden to the queens they cast, the community they serve, and focus on the contest itself rather than choosing fairweather political allies and lookie-loos and homogenizing drag at the expense of its political punch.
The success of Heated Rivalry has brought up an interesting question: is the fact that these two sexy hockey players are fundamentally unavailable the secret to their forming a deeper, meaningful relationship? Is the possibility of intimacy and romance based on the fact that they can’t have it?
Sure, that’s fiction, but after my breakup with an aspiring “poly” Scorpio with an avoidant attachment style, I spent a year being a fuckboy. I thought growing out my beard was a game-changer, but being emotionally unavailable was like having three dicks. Having no interest in a romantic connection somehow made it so much easier to get laid, meet guys, and connect without running the risk of sabotaging things.
I was shocked by how much attention I got. It’s like guys could smell the unavailability, and it fueled me having connections more deeply than when I was available. I’ve always struggled with the idea of playing hard to get. Why would I pretend I don’t like someone? Isn’t that lying?
And yet, it seems like that is the secret of success. I was recently reconnecting with a guy. We had a ton of great chemistry, common interests, and were really excited to get together. He was sick, so we couldn’t hang out. My eagerness to meet may have gotten the best of me because rather than finally meeting, he broke things off, saying he wasn’t ready for anything deeper.
As I switched from being emotionally unavailable to primed to date, I lost all of my emotionally unavailable powers. I even had to ask myself if I had fallen into the same trap. Was I so attracted to him because he was definitely not a love match? Why do we constantly seek out people who are unavailable?
Sometimes, you have the freedom to really let yourself go and put down all your walls because you know subconsciously there are no stakes because the relationship has an expiration date. It reminded me of a conversation I had with a friend.
He had hooked up with someone on a boy’s trip and was lamenting that this guy, who already had a partner, did not have the same feelings. We had a long conversation from NorCal back to Los Angeles reflecting on attachment styles, romance, and our longing for connection.
Then our friend broke all of our brains. He asked if he was addicted to the feeling of longing. That exciting feeling you get from someone new. He pointed out, what if on some level my friend was not just attracted, but dare I say attached, to the feeling of fundamentally getting rejected?
You can’t look at gay relationships and not think of trauma. On some level, the decision to pursue your same sex attraction comes with the potential to be voted off the island. In extreme cases, you get thrown out of your house. Your relationships can change, leaving a rejection wound that we like to pick at every time we date some fuckboy, guy with a partner, or someone who is fundamentally bad for us.
Our community is a bit like the Wild West. You can end up on the wrong side of someone’s unresolved issues with their family, sexual assault trauma, or the bad karma of their past relationships. Gay men are trauma survivors who can traumatize each other.
Our dating pool is also our pool for friends, rivals, business contacts, and romantic partners. And yet, why is it that the people who are unavailable, like cream or scum, rise to the top? Is the allure of the unavailable the retraumatization of our messy familial relationships? Is it revisiting the longing of our queer awakening for that first guy who didn’t choose us? Are we chasing some initial early wanting we developed in the closet?
Are we chasing the fantasy of love and projecting that onto some guy who feels ambivalent to us? It’s worth asking these questions because if we look at our friend groups and dating histories, charting the complex boundaries and intermingling connections is like watching a Ryan Murphy show with better writing.
But it goes deeper. Are we sabotaging relationships by rejecting people who like us? After all, as men, it’s not unheard of to have a bit of a fear around intimacy and vulnerability. There’s also the fundamental scientific and economic concept that scarcity equates to value. So do we chase someone who has a greater premium on their time and attention?
As queer men, we hack our bodies to get in better shape, and many of us do that with our relationships. We end up forming a complex system of fuck buddies, situationships, intimate platonic friends, and crushes, forming a distorted jigsaw puzzle that forms the equivalent of one relationship. Meanwhile, what would it be like exploring what it would be like to just spend time with one person and then putting them back in the pond for someone else?
There are men in open relationships who spend more time in the pursuit of sex and male attention than single folks. There are friends who use their friends’ unresolved sexual or romantic feelings to have their intimacy needs met while playing the field.
This could just be the nature of city-dwelling gays in a city like Los Angeles. After all, to have countless options, guys end up with an ever-growing list for Santa of the man who’s “worth” settling down for.
Can we just appreciate when someone likes us? How can we focus on the positive and support a queer brother who, despite all the political fuckery of our society, still has the confidence to put themselves out there and choose love? Can we reject without crushing someone’s spirit or introducing unnecessary drama?
What if we love ourselves enough to realize we deserve love and the people we’re with to love us back?
Can we not put undue pressure on the men we fancy to not just be the object of our affection but the sum of all of the things we’re not dealing with, the solution to our unreseolved childhood romantic feelings, and fulfilling an ever-evolving fantasy?
At the end of the day, we have to all realize we are all people who have more in common than we have differences, stop projecting our problematic pasts or hopes for the future onto each other, and learn a little bit about how to love better. That way, we can be present with the people we are with rather than cast them in roles in the soap opera in our heads.
While your straight friends assume you’re having sex all the time, let’s be honest, you aren’t having as much as you’d like. It begs the question: Are you even satisfied with the sex you’re having? Is it because of how much we sacrifice to get laid?
While technology has made sex like ordering a pizza, there are a certain set of personal sacrifices that we’re being charged to scratch that itch.
The strange mingling of intimacy and the transactional nature of consumerism crosses a line we may not be able to come back from. You end up with insatiable cock goblins and people negotiating intimate encounters like a business deal.
Apps make it easier than going out to get some, and yet, we end up disembodied body parts talking to each other like animals. We sacrifice our humanity and our expectations of respect. Why should straight people get the HR-friendly polite treatment, and then you treat someone you will have inside you or be inside like shit for wanting exactly what you want?
We have this strange cultural norm of getting penalized for exhibiting interest. The internalized homophobia programmed so deeply with the fear of intimacy, the rejection of homosexuality that we punish people for expressing interest. We’re encouraged to feel less than, or wonder if we’ll ever be loved.
Hurt people hurt people, so we end up in a culture where we’re swapping traumas and battle scars like we’re playing Pokémon. How often do you leave an interaction or relationship feeling worse? Why must we lose peace in service to a moment of pleasure?
Must we sacrifice some of our authentic selves to be the performative masculine stud men want?
Must we become inhuman testosterone-fueled beasts, more forgiving of disrespect to navigate the Wild West that is app culture? Now, with the push of a button, you can make a total stranger feel like shit because you had a bad day? You hate your father? You were assaulted, or you’re feeling insecure?
Many men have a separation of church and state between the version of themselves you meet in their personal and even romantic lives and the bedroom. They play some role in the bedroom and turn off their brain. Slide Tab A into Slot B like putting together Ikea furniture with the same amount of boredom and routine.
It can take years of inner work to integrate the person you are when you have sex with the man in the streets. Sex becomes a means to an end rather than the connection of two bodies, two people. After all, when you’re hooking up with a stranger, you’re often making up the rest. But when is it too far? How much of ourselves must we give up to get some?
I pride myself on being the same guy you meet in a social setting, at work, and when I’m having sex. Could the popularity of cum dumps, hookup apps like Sniffies, be that we aren’t getting what we want from sex without strings? There may not be a lasting connection, and yet there is something that lingers.
Before you check out, I am not presuming the right answer is a husband, kids, and a picket fence. But I wonder if the reason we are seeking so much sex is that we’re trying to recoup the effort we put in.
Throughout queer history, I’ve heard it’s Manhunt. What do you expect? It’s Grindr. What do you expect? It’s Sniffies, what do you expect? I would expect someone who knows how much it hurts to not be a dick?
And yet the tech wizards are engineering new ways to make the process faster. We settle for a collection of quasi-relationships rather than finding a connection. Do we need to become sex crazed demons or avatars for porn-style fantasies?
We end up touch-starved and checking the apps like stock portfolios, sacrificing our safety, emotional well-being, humanity, or romantic goals. What if the solution is just compromise, kindness, and seeking some sort of brotherhood?
While some people can have a casual sexual encounter and use the commingling intimacy to be friendly, connect, and establish a friendship or aquiantenship others can have a delightful encounter and then block you.
I’d like to think that the sacrifice we should be making is checking the parts of ourselves we still keep in the closet: the shame, trauma, sublimated anger, and thirst for destruction, and not make that someone else’s problem. What if we save that dark energy to fight back and fight for our community?
What if we focused on the fact that we all know what it’s like to like someone who doesn’t like us back, to get cancelled at the last minute, and to just want a moment of post-nut clarity? Hopefully, rather than make it “easier’ and faster to get laid, we can all just make it a little bit easier to be a queer person in this crazy world by helping each other find joy inside and outside the bedroom.
COMMENTARY
If you’re exhausted from dating in 2025, this is how you restart for 2026
What are you going to do differently this year?
If you ended last year feeling like you’ve dated everyone, tried everything, and there’s no one left, I want you to pause for a second because that feeling is incredibly common, especially for gay men.
So let me ask you something, honestly.
What are you going to do differently this year?
Are you just going to get back on the apps again?
Back on Grindr.
Back to the same bars.
Same patterns. Same guys. Same conversations.
And hope somehow this year turns out better?
If you change nothing, nothing changes.
A lot of men I talk to are stuck in this back and forth. Do I want a relationship, or do I just want something casual? Am I ready? Is the timing right? Should I focus on dating or my career? Do I have enough money saved? Am I far enough along in life?
That constant indecision keeps you stuck right where you are.
Then we pile on old rejection, trauma from growing up gay, low self-esteem, and suddenly we start believing we need someone hotter than us, richer than us, more put together than us to feel chosen.
But here’s the part I want you to really hear.
You don’t fall in love with a checklist.
You fall in love with how someone makes you feel.
Do they make you feel safe?
Do you feel calm around them?
Do you feel seen?
Do you laugh together?
Do you feel good being yourself?
That’s what actually builds connection.
Money doesn’t do that.
Abs don’t do that.
A job title doesn’t do that.
Those things can change. They come and go.
So here’s where I’m going to point the finger back to you, in a loving way.
If you’re clear on the kind of man you want, what are you doing to become closer to that person yourself?
If you want someone kind and generous, how are you practicing kindness and generosity in your daily life? Do you volunteer? Do you compliment the person standing next to you even when there’s no attraction? Do you lead with warmth or with judgment?
If you want someone who values family, how much time are you actually spending with yours? Do you prioritize relationships the way you want someone else to?
If you want someone with a full life, hobbies, passions, and friends, what does your life look like right now? Are you doing the things you say you want to do, or are you sitting on the couch thinking about them? You want to play piano. Travel. Hike. Be more active. What steps are you taking to actually live that life?
If you want someone active and adventurous, are you active and adventurous? If you want someone calm, grounded, and emotionally steady, how are you working on becoming grounded yourself? Do you meditate? Do yoga? Take some quiet time? Do anything that regulates your nervous system?
How about finding someone with an amazing body? How does your body look? Are you working out and eating well yourself?
By the way, you can always help your partner get into healthier habits if you are practicing them yourself.
This isn’t about perfection. It’s about alignment.
If you’re expecting someone to check every box while you’re not checking those boxes yourself, that’s not standards. That’s unrealistic expectations.
And remember, our dating pool is already small. Roughly four percent of the male population identifies as gay, bi, queer, or trans. Cut that down to people who are single. Then emotionally available. Then compatible. Then sexually compatible.
The number gets smaller fast.
So maybe this year we stop being so rigid.
Maybe we loosen the rules a little.
Maybe we focus less on the perfect body and more on the right energy.
Chemistry usually doesn’t show up on the first date. Most of the time it doesn’t. So if there’s even just a little attraction, kindness, and curiosity, maybe give it a second date. Maybe slow down long enough to actually see who’s in front of you.
Doing the same thing over and over is not dating. It’s just repeating patterns.
Dating with intention means being honest with yourself first.
If this year you’re ready to stop guessing, stop burning out on apps, and actually have a plan, matchmaking can help. You don’t need more options. You need clarity, accountability, and guidance from someone who understands queer dating and knows how to help you show up as your best self. If you’re serious about doing things differently this year, that’s where matchmaking comes in. Click here and let’s start 2025 right.
Daniel Cooley is a gay matchmaker & co-owner of Best Man Matchmaking – California’s premier service for queer and trans men seeking emotional connections. Learn more here.
Commentary
Trump’s triple X testosterone crusade to capture the Western Hemisphere
Veteran journalist and LGBTQ+ ally Lucian Truscott IV analyzes Trump and the Venezuela invasion
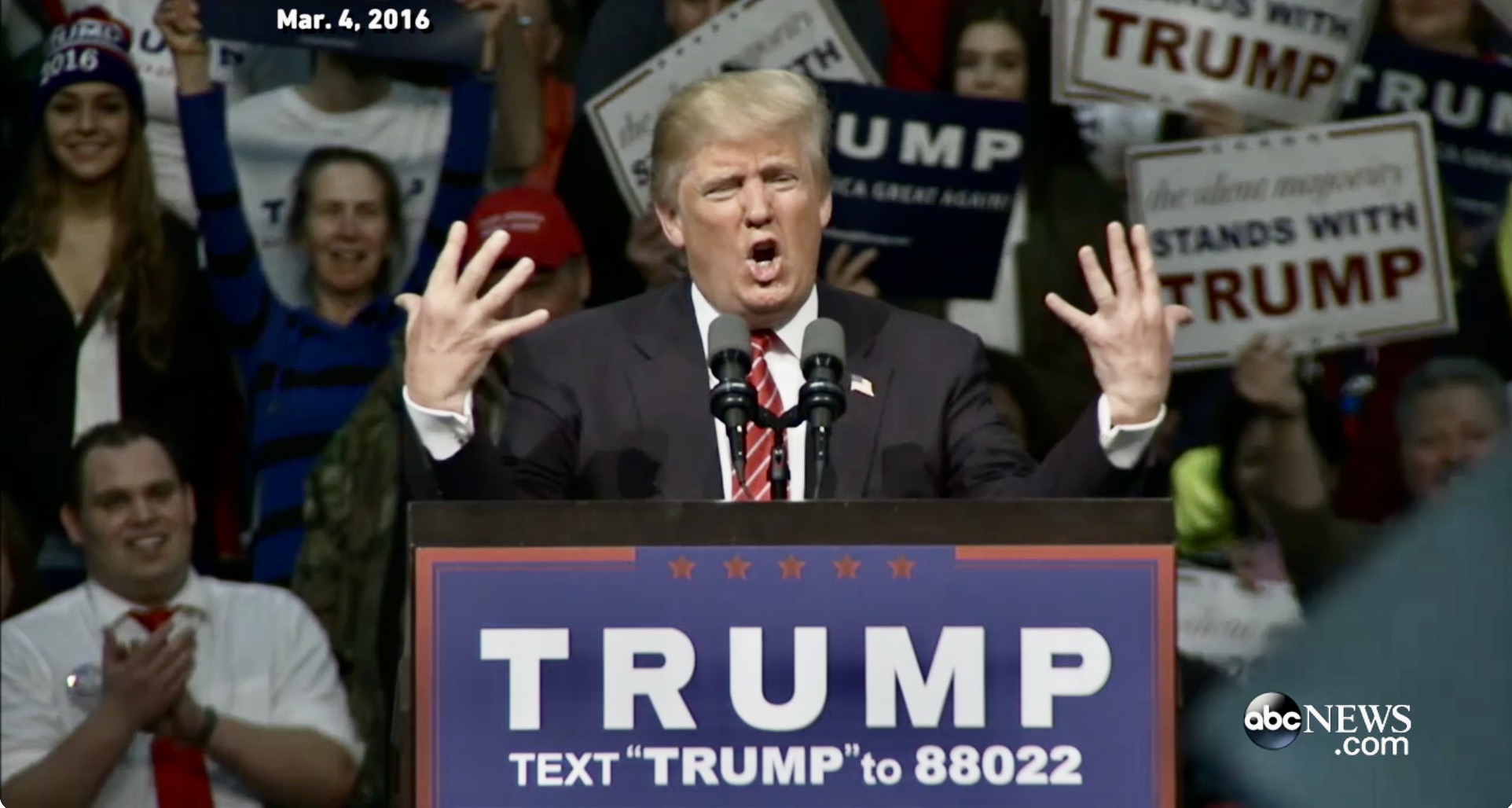
No one’s talking about Donald Trump’s small hands now or his low poll numbers or affordability failures or the 5.2 million unreleased Epstein files or the testimony of former Trump Special Counsel Jack Smith on the 5th anniversary of the Jan. 6 insurrection – not after the U.S. unleashed a surprise shock and awe bombing campaign in Venezuela on Friday night, Jan. 2. With great military precision, the United States successfully kidnapped Venezuelan President Nicolás Maduro and his wife Cilia Flores without the loss of any American lives.
Apparently, the 80 people who were killed – including civilians, Cuban nationals, and some Venezuelan military –are insignificant collateral damage.
A moment after the decapitation of leadership settled in, some Venezuelans celebrated the end of Maduro’s brutal reign of power. But Trump swiftly snatched away joy, announcing that “we are going to run the country,” along with Maduro’s former vice president, who was threatened into accepting the interim presidency to stabilize the transition to whatever Trump wants next in this sovereign country and to facilitate oil transactions. There is some confusion about the loyalty of the rest of the intact Maduro regime and the reaction from opposition activists.
What does that mean for someone like Andry José Hernández Romero, the gay stylist who fled Venezuela after being persecuted for his sexual orientation and open opposition to Maduro? Though he complied with all requirements to seek asylum in the US, he was arrested and, without due process, was deported with 250 other Venezuelans to the horrendous torture prison CECOT in El Salvador, where he suffered daily assaults and abuses.

“We were lied to by ICE officials and then greeted in CECOT with beatings,” said Romero after he was sent home. “At every step of the way, they abused us. But being Venezuelan is not a crime. I’m grateful to Congressman Takano who has called for justice for the 252 Venezuelan men sent to CECOT without the opportunity to present their case in immigration court.” Questions about how and why so many amoral violations of due process took place are still on hold.
Trump’s second term is all about toxic performance masculinity, and following up bellicose bluster with actual brute force. Secretary of Defense Pete Hegseth’s Pentagon has murdered more than 100 people aboard alleged drug smuggling boats blown up by drones as if in a video game. The UN calls the killings “extrajudicial executions” since the US has produced no evidence or allowed due process to contest the claims that the boats were hauling fentanyl for distribution in the United States.
Oddly, the Pentagon has not released video of the blowing up of two survivors of a strike, clinging to a piece of wood for 45 minutes before they, too, were blown up Sept. 2 by a plane they apparently thought might rescue them.
It’s all about the drugs, say Trump acolytes, as if that balances out the inhumanity. Attorney General Pam Bondi provided a new 25-page indictment charging Maduro with heading a transnational narco-terrorist organization along with his wife and son. Secretary of State Marco Rubio, who has been pushing for regime change in Venezuela, described the attack as a “law enforcement” operation, without the need for Congressional advice and consent.
But the US indictment against Maduro cites cocaine, not fentanyl, which is “almost entirely produced in Mexico using chemicals from China,” according to U.S. authorities. “Venezuela plays no known role in its trade, nor does any other South American country,” the New York Times reports.
Venezuela is a pass-through country for cocaine. Meanwhile, in 2022, the U.S. attorney’s office for the Southern District of New York charged ex-Honduran President Juan Orlando Hernández with “one of the largest and most violent drug-trafficking conspiracies in the world,” responsible for the “unfathomable destruction” cocaine had caused in the United States.
Hernández was abruptly pardoned by Trump last month. “The man that I pardoned was, if you could equate it to us, he was treated like the Biden administration treated a man named Trump,” Trump told The Times, adding, “This was a man who was persecuted very unfairly. He was the head of the country.”
Trump seems addicted to unabashed lying. The Washington Post Fact Checker team found that Trump’s false or misleading claims totaled 30,573 over his first four years in office, “averaging about 21 erroneous claims a day.” On July 07, 2025, Yale experts released their findings on Trump’s claims or assertions. “Artificial intelligence discredited all the Trump claims we presented, fact-checking the president with startling accuracy and objective rigor,” they reported.
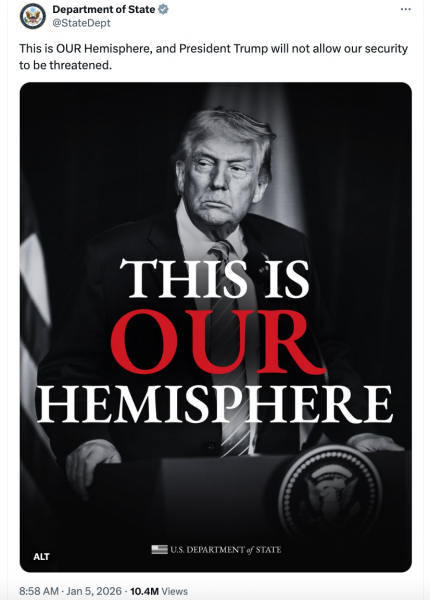
Trump demands that loyalists buy into his lies and bellicosity – including the latest, claiming Western Hemisphere domination. Rubio is salivating over destroying Cuba, as giddy as when he dreamed of besting his GOP rival in 2016.
“He is taller than me, he’s like 6’ 2”, which is why I don’t understand why his hands are the size of someone who is 5’ 2”,’ Rubio joked. “Have you seen his hands? And you know what they say about men with small hands – You can’t trust them,” ABC News reported.
Trump flipped the script on this manhood vulnerability, convincing the crowd they weren’t seeing what they were seeing. “Are they small hands? And he referred to my hands — if they are small, something else must be small. I guarantee you there is no problem. I guarantee you.” (Fact check: porn star Stormy Daniels says Trump’s penis is like “a toadstool.”)
Remember those small hands when Trump talks about going into a sovereign country to get oil, or Deputy Chief of Staff Stephen Miller talks about annexing the Danish territory of Greenland. There’s a smirky sexual overcompensation infused with the presumption of power.

“We live in a world in which you can talk all you want about international niceties and everything else, but we live in a world, in the real world, Jake, that is governed by strength, that is governed by force, that is governed by power,” Miller told CNN’s Jake Tapper on Monday. “These are the iron laws of the world since the beginning of time.”
Sounds like Trump’s reply to E. Jean Carroll’s out lawyer Roberta Kaplan during his 2023 deposition.
From CNN transcript:
KAPLAN: And you say – and again this has become very famous – in this video, “I just start kissing them. It’s like a magnet. Just kiss. I don’t even wait. And when you’re a star, they let you do it. You can do anything. Grab them by the p*ssy. You can do anything.” That’s what you said. Correct?
TRUMP: Well, historically, that’s true with stars.
KAPLAN: It’s true with stars that they can grab women by the p*ssy?
TRUMP: Well, that’s what, if you look over the last million years I guess that’s been largely true. Not always, but largely true. Unfortunately or fortunately.
KAPLAN: And you consider yourself to be a star?
TRUMP: I think you can say that. Yeah.”
Grabbing Venezuela’s oil or Greenland’s potential wealth of critical minerals is the rape of someone else’s land. As Trump’s testosterone-related lawsuits suggest, he’ll need a lot of money and backup to get away with it.
I called my friend Tom Carpenter, an attorney and Marine Corps Captain and Naval Academy graduate who chaired Servicemembers Legal Defense Network, for his thoughts on what’s happening – might there be a draft to cover all the invasions Trump’s threatened? Tom said he’s following his friend – West Point Academy graduate Lucian K. Truscott IV – a straight man in the alum’s gay Knight’s Out association – whose Substack is erudite, illuminating, and funny.
Case in point: “Boy, are the think tank and media foreign policy poohbahs stumped after Trump’s big kidnapping of Mr. and Mrs. Maduro on Friday night. All of them agree that it was a brilliant military operation, which Secretary of State Marco Rubio insists on calling a law enforcement ‘mission in support of the Department of Justice.’ Which I guess isn’t that far-fetched a description, given the fact that we have platoons of armed, uniformed men in full combat gear running around our own country conducting Gestapo-like law enforcement missions on unsuspecting people, immigrant and citizen alike, as they go about their business of living peaceful lives in the United States of America.”

In Trump’s plan for Venezuela: A hope, a prayer, and golf, Lucian also noted in a White House photo that a waiter stood behind Trump, Rubio, and CIA Director John Ratcliffe in a makeshift ballroom/sit-room watching the assault. “Trump couldn’t inform Congress, but if you were a Mar-a-Lago waiter on Friday night, you knew everything that was happening in Venezuela in real time.”
Lucian comes from a long line of Army heroes: his father was an Army colonel who served in Korea and Vietnam; his grandfather, Lucian Jr., was a U.S. Army general during World War II, commanding the 3rd Infantry Division and later the Fifth Army in Italy. Lucian attended West Point, graduating in 1969, but not before causing some “good trouble,” which we discuss in our Zoom conversation.

A journalist and author, one of his books, Dress Gray, is about the murder of a gay cadet. In 1986, it was adapted for the screen by Gore Vidal and made into a TV miniseries that aired on NBC March 9–10,1986.
Lucian is also a descendant of American Founding Father Thomas Jefferson and created some controversy by inviting the descendants of Jefferson’s enslaved mistress, Sally Hemings, to a 2000 family reunion.
But among LGBTQ+ historians, Lucian is perhaps best known as the first eyewitness reporter, along with gay columnist Howard Smith, his colleague at the Village Voice, to cover the riots at the Stonewall Inn, published July 3, 1969.
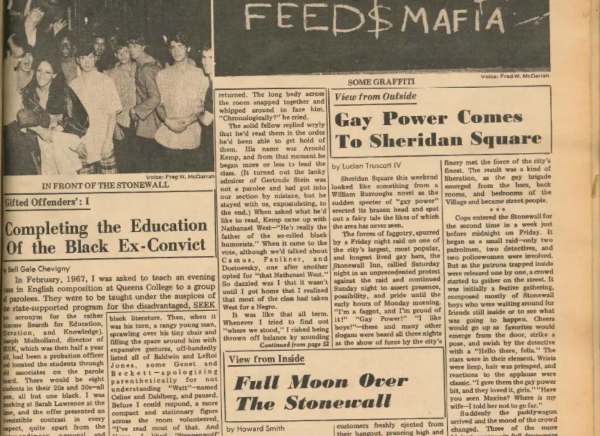
“Sheridan Square this weekend looked like something from a William Burroughs novel as the sudden specter of ‘gay power’ erected its brazen head and spat out a fairy tale the likes of which the area has never seen,” Lucian wrote, opening a very detailed account, laced with words like “faggot” and “dyke,” commonly used language at the time. Lucian later wrote that a protest led by Jim Fouratt over the slurs prompted Lucian and the Village Voice to change their language.
Importantly, Lucian writes with specificity about that night on June 28, 1969 – including: “The next person to come out was a dyke, and she put up a struggle — from car to door to car again. It was at that moment that the scene became explosive. Limp wrists were forgotten. Beer cans and bottles were heaved at the windows, and a rain of coins descended on the cops.”
Two nights later, Lucian hangs out with famed gay Beat poet Allen Ginsberg. “Gay power! Isn’t that great!” Allen said. “We’re one of the largest minorities in the country — 10 percent, you know. It’s about time we did something to assert ourselves.”

Lucian accompanied Ginsberg into the Stonewall Inn, which was blaring with rock music, and later walked him home. “Along the way, he described how things used to be. ‘You know, the guys there were so beautiful — they’ve lost that wounded look that fags all had 10 years ago.’ It was the first time I had heard that crowd described as beautiful.
“We reached Cooper Square, and as Ginsberg turned to head toward home, he waved and yelled, ‘Defend the fairies!’ and bounced on across the square. He enjoyed the prospect of ‘gay power’ and is probably working on a manifesto for the movement right now. Watch out. The liberation is underway,” Lucian wrote.
In our Zoom conversation, we talked about Trump, Venezuela, how Trump’s ludicrous dreams of imperialism could defeat him, Sen. Mark Kelly, a possible draft, and so much more. I also asked Lucian why he is an LGBTQ+ ally.
“That’s the kind of thing I learned from my parents and from my mother, from my grandmother – was you disarm people with humanity. That’s what you do. If you’re a human being, act like one,” Lucian K. Truscott IV said. “And if you act like one, eventually, once you brush things and clean crap off your feet like Donald Trump – you win… So I guess my message is: it’s not going to be easy – but this, too, will pass. It will.”
It’s our job to hasten the passage.
This is a cross-post from Karen’s LGBTQ+ Freedom Fighters Substack. Please enjoy the video conversion with Lucian K. Truscott IV on the site and check out his daily Substack.
-

 Arts & Entertainment2 days ago
Arts & Entertainment2 days ago2026 Best of LGBTQ LA Finalist Voting
-

 Health3 days ago
Health3 days agoWhere medicine meets dignity: Be Well Medical Group founder Isaac Berlin is here and queer to serve the community
-

 Out & About3 days ago
Out & About3 days agoQueer, trans AAPI joy shone at this year’s Golden Dragon Parade
-

 Mexico4 days ago
Mexico4 days agoUS Embassy in Mexico issues shelter in place order for Puerto Vallarta
-

 Commentary2 days ago
Commentary2 days agoWhen optics matter more than harm: BAFTA, BBC, and editing solidarity while letting slurs slide on through
-

 California2 days ago
California2 days agoExperts discuss pathways forward as anti-trans violence continues to rise
-

 Autos3 days ago
Autos3 days agoGoing for gold: Ford Bronco Sport vs. Toyota RAV4
-

 Books2 days ago
Books2 days agoNew book profiles LGBTQ+ Ukrainians, documents war experiences
-

 a&e features2 days ago
a&e features2 days agoRevry Co-Founder Damian Pelliccione on why we need ‘King of Drag’
-
 Books1 day ago
Books1 day agoThe social side of self-pleasure: Artist Jason Wimberly presents his newest book of photography, HOMOSOCIAL








