Health
1 in 4 LGBTQ youth identify as nonbinary, half also identified as Trans
Asked about ways others can make them feel happy- nonbinary youth overwhelmingly responded: having people use the correct name & pronouns

NEW YORK – In a study released to mark International Nonbinary People’s Day on Wednesday, the Trevor Project published new research on the diversity of nonbinary youth. The report sheds light on the nuances of youth gender identity, pronoun usage, the consistency of nonbinary identity across race/ethnicity and age, as well how to implement better support for nonbinary youth mental health.
“Young people are using a variety of language to describe the nuances of their gender identity outside of the binary construction of gender. These data emphasize that, while there is certainly an overlap, youth understand ‘transgender’ and ‘nonbinary’ as distinct identity terms — and you cannot assume one’s identity simply based on the pronouns they use,” said Jonah DeChants, Research Scientist for The Trevor Project.
“These findings emphasize the need for policies that affirm nonbinary youth in their identities, such as respecting their pronouns and allowing them to change their name and gender marker on legal documents like driver’s licenses and birth certificates. Being that something as simple as respecting pronouns can be life-saving, we must work to expand training and improve understanding of transgender and nonbinary identities among schools, medical facilities, and youth-serving organizations and adults,” he added.
Key Findings:
- One in four LGBTQ youth (26%) in our sample of nearly 35,000 identified as nonbinary. An additional 20% reported that they are not sure or are questioning if they are nonbinary.
- While nonbinary identities have often been grouped under the umbrella term of “transgender,” our data show that only 50% of youth who identified as nonbinary also identified as transgender.
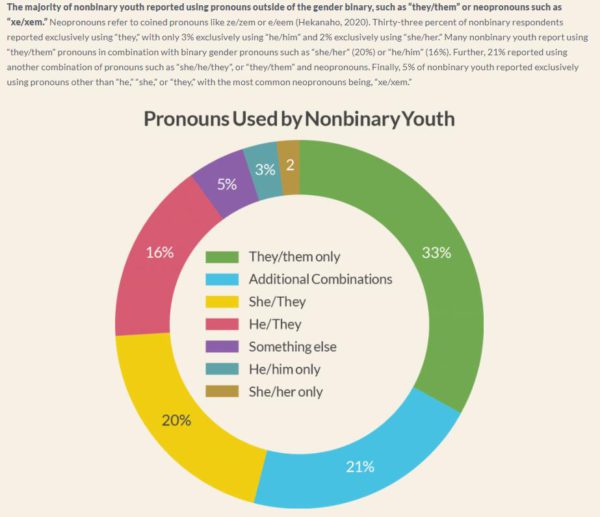
- The majority of nonbinary youth reported exclusively using pronouns outside of the gender binary, such as “they/them” (33%) or neopronouns (5%), such as “xe/xem.”
- When asked about ways other people can make them feel happy or euphoric about their gender, nonbinary youth overwhelmingly responded: having people in their life use the correct name and pronouns to refer to them.
- Nonbinary youth who reported that “no one” respected their pronouns had more than 2.5x the rate of attempting suicide compared to those who reported that “all or most of the people” they know respected their pronouns.

Related to Wednesday’s International Nonbinary People’s Day celebrations and the Trevor Project Study findings, PFLAG National Executive Director Brian K. Bond told the Blade in an email; “Parents and families seeking resources and answers when a loved one comes out as nonbinary find that support and more with their local PFLAG chapter. PFLAG National and the entire PFLAG Chapter Network celebrate and affirm you, on International Nonbinary People’s Day, during Nonbinary Awareness Week, and year-round.”
Resources for PFLAG’s efforts are here: pflag.org/nonbinary-resources.
LGBTQ+ Youth Mental Health
For queer youth, LGBTQ+ scholarships affirm their visibility and sense of possibility
The Blade spoke with student advisory council members from the National Rainbow College Fund, which provides funding and community-building for LGBTQ+ students and allies.

Bey Michael Madden describes their queer identity as a “difficult journey.” They trace the start of that winding path to the small town in Pennsylvania they grew up in, and how they weathered isolation by slowly learning how to care for themself. Today, Madden works at a nonprofit that supports people transitioning from homelessness and dealing with the aftermath of trauma. “I help folks…take those experiences and turn them into medicine,” Madden told the Blade.
Madden is currently studying social work and psychology, with the hopes of becoming a therapist who can continue to support marginalized community members and fellow queer people. They are a scholarship recipient of the National Rainbow College Foundation (NRCF), and currently serve on the organization’s student advisory council.
The NRCF, and the nonprofit Madden works at, imbues them with a sense of purpose and fulfillment. It also provides them with tangible support to manifest their dreams in an educational, political, and social landscape that presents various obstacles and barriers for queer people.
In 2021, Williams Institute researchers found that over half of transgender adults, as well as 35.9% of queer women and 27.9% of queer men, have federal student loans — making LGBTQ+ adults and students more likely than non-LGBTQ+ people to accumulate debt over their studies. For many, this kind of financial burden is untenable.
“Growing up, my parents would not have been able to help support my college journey…[They] work, day and night, trying to help not only me, but also my sisters,” said Abril Colin, another member of NRCF’s student advisory council. Colin studies nursing and is determined to make healthcare spaces more inclusive and welcoming for queer folks and Latine people. As a child, Colin had to translate for her parents during doctor’s appointments, intimately understanding systemic gaps that make it difficult for marginalized people to seek the support they need.
NRCF makes these goals feel more accessible. Since 2024, the organization has provided scholarships for nearly 200 LGBTQ+ students — regardless of whether or not they are publicly out. This year, they will support another 200 students with $2,500 each. Additionally, the NRCF is exploring ways to deepen community amongst their scholarship recipients, and provide them mentorship and training on personal development, leadership skills, and ways to seek out more opportunities at their respective schools.
“Without this kind of support, I feel like a lot of queer people are left at the sidelines, watching others succeed and not knowing if they can access that success on their own,” Madden said.
Jorge Bernal understands the weight of this “unknowing,” having spent his childhood in the Imperial Valley’s foster youth system. “I didn’t have any familial support, and it was hard to grow up, identify on the LGBTQ+ spectrum [and go] to college myself without any [help],” Bernal said. With the support of NRCF, he is able to explore his interests in environmental science, and hopes to eventually return to his hometown to affect change in soil practices and decrease respiratory health issues within his community.
This sense of service and intentional exploration is ample in the student advisory council, many of whom are young and experiencing formative queer firsts.
“[What] I really love about these kinds of programs that are propelling LGBTQ youth and communities, is that it’s really [about] building spaces where we can be ourselves and celebrate each other,” said Samantha Rivera, who is studying law, public policy, and society. “That’s something I experienced for the first time very recently,” she continued, recounting a banquet she attended that was celebrating queer people.
“That was so cool, and something I had never experienced before. That really is something you can get by applying [to programs like NRCF],” Rivera said, who, like many other queer students, is grounded by her intersectional identity and her deep ties to the people and places that have allowed her to embrace these facets.
“It’s building community [and making] sure everybody’s safe in their own shoes and skin,” reiterated Saivionn Williams, another student advisory council member. Williams is studying abroad in Spain, where he is witnessing queer communities in a different cultural context.
Considered one of the most LGBTQ+ friendly countries in the world, Spain has offered Williams a glimpse into a different queer ecosystem and a new kind of hope for his own home. “[Spain is] more accepting, laid-back, and communicative. I do believe the U.S. has it deep inside [to be the same]. Maybe not this year, but we are taking steps forward as a community to reach that point.”
To reach a point where queer people and youth are prioritized and protected, organizations like the NRCF are nurturing voices that face mainstream vilification. With recent comments made by both President Trump and Governor Newsom, who respectively decried trans rights and criticized “identity politics,” this direct pathway for LGBTQ+ student funding is, in its own way, a form of queer resistance and empowerment.
This year’s National Rainbow College Fund scholarship deadline is Mar. 4 at 2 p.m. PST. It is open to students in California, and selected recipients will be awarded $2,500 as well as opportunities for community, resource sharing and skill-building. More information can be found here.
Kristie Song is a California Local News Fellow placed with the Los Angeles Blade. The California Local News Fellowship is a state-funded initiative to support and strengthen local news reporting. Learn more about it at fellowships.journalism.berkeley.edu/cafellows.
Commentary
When optics matter more than harm: BAFTA, BBC, and editing solidarity while letting slurs slide on through
A polite examination of where priorities lie when the BBC chooses to censor political solidarity yet allows a racial slur to air unedited, and what this might say about the industry as a whole

The night was meant to be a celebration. At the British Academy Film Awards, an institution that claims to pride itself on honoring the best in international cinema, the cast and creatives of Sinners arrived as nominees, as artists, as guests. Instead, they were confronted with a word that should have no oxygen left in public life.
On stage, actors Michael B. Jordan and Delroy Lindo were visibly jarred. You could see it flicker across their faces, the moment when shock and dismay meet recognition. And yet they both proceeded unflinchingly with grace and poise, because that is what Black people so often have to do to keep progress progressing. Tough skin. Resilience. Smile through it. Keep it moving.
But what is undeniable is the weight. The weight that that particular slur carries, especially when it comes from the mouth of a white person. It carries centuries of hate, atrocities, and trauma. It echoes lynchings and segregation, caricatures and exclusion. It is one of the most violent linguistic relics in the English language, and it is an undeniable trigger, a generational trauma that continues to afflict an entire demographic of the population. There is no casual context in which it lands softly, and no stage vast or shiny enough to dilute its history.
BAFTA eventually apologized. Too little, too late. This is your stage, and these are your guests. It is your responsibility to protect and advocate for them in the moment, not hours later when headlines begin to circulate. Award shows have removed attendees for far less. If a guest shouts a bomb threat, if someone storms the stage, or if there is a physical altercation, swift action follows. Why, then, does a quintessentially racist slur prompt hesitation? Why is decorum preserved more urgently than dignity?
Complicity is far too telling, and passivity is far too common. When celebs like Neil Patrick Harris retreat behind tiresome labels of “apolitical,” what they are really aiming to guard is not neutrality but comfort. As a gay white man, Harris exists in a space where his privileged identity eclipses his marginalized identity. His queerness can be selectively foregrounded, while the protections afforded by his whiteness shield him from realities faced by communities who wear their otherness on their skin. This insulation Harris possesses makes silence that much more palatable to his tongue.
Hollywood no doubt understands the power of narrative control better than any industry. Edward Bernays, the nephew of Sigmund “Uncle Sigi” Freud, built the blueprint for modern propaganda by teaching institutions how to shape perception, manufacture consent, and quell public outrage. That legacy of image management continues today with folks like with Netflix co-founder Marc Randolph, Edward Bernays’s own nephew (runs in the family). The industry knows how to redirect attention, isolate incidents, and reframe harm as a simple and easily forgivable and forgettable misunderstanding.
Back to the BAFTAs, I understand that John Donovan lives with Tourette’s syndrome, and that tics are involuntary. This reality deserves full acknowledgment. Neurological conditions are not punchlines, nor are they moral failings. But accountability and accommodation can coexist. One question remains conspicuously unanswered in much of the coverage: did Mr. Donovan, as “mortified” as he claims to have been, immediately excuse himself from the room? Did he remove himself from the space as soon as the word left his mouth? Or were his apologies as delayed as BAFTA’s?
Too many are quick to reduce the entire incident to a diagnosis, as though that ends the conversation. If this grown man is of sound mind enough to create and promote a film about his experience living with Tourette syndrome, then surely he is also capable of understanding the magnitude of that word and the necessity of immediate harm mitigation. A condition may explain behavior. It does not erase impact. It does not absolve institutions from responding decisively.
Coverage has framed the moment as an isolated incident during the awards ceremony. But Sinners production designer Hannah Beachler tells a different story. “I keep trying to write about what happened at the BAFTAs, and I can’t find the words. The situation is almost impossible, but it happened three times that night, and one of the three times was directed at myself on the way to dinner after the show.”
Three times.
Why, then, is most coverage focusing solely on the on-stage incident? Because that one was caught live, in front of cameras, in front of an auditorium of witnesses. It is easier to contain a scandal to a single viral clip than to interrogate a broader culture. But if it happened three times in one evening, the problem is an environment, not a single tic-induced outburst. Again, BAFTA, who are you letting into the party? What safeguards are in place? What standards are enforced when the cameras are off, and the ancillary festivities and dinners begin?
One glaring example of misplaced priorities came when the BBC chose to edit out filmmaker Akinola Davies Jr’s call to “free Palestine” from its televised BAFTA coverage, while simultaneously failing to remove the audible racial slurs. Folks couldn’t help but take notice that both decisions happened within the same two-hour tape-delayed broadcast window, yet the network found time to censor a politically charged solidarity statement while allowing the slur to slide through unscathed. This discrepancy raises questions about what content editors deem unacceptable versus what they allow to reach millions of viewers. The caucacity is truly mind-boggling and blood-curdling.
The fact that this occurred on such a prestigious platform in 2026 and was met with delayed apologies that skirt clear culpability is precisely why Black history cannot remain a neatly packaged 28-day-long pat on the back. It must be in the curriculum in schools. It must be contextual in conversations. It must be uncomfortable because it is necessary. Because when people understand the lineage of that word, its architecture of harm, its function as a weapon, maybe, just maybe, they will treat it as such.
This isn’t about political correctness. It is a matter of institutional responsibility and whether global stages will continue to rely on the grace of Black artists to absorb humiliation in real time. Progress does not sustain itself on resilience alone. It requires intervention and accountability. And sometimes, it requires cleaning house before you roll out the red carpet again. Michael B. Jordan and Delroy Lindo, you two kings have stoicism and poise that far surpass my own. That said – Take a seat, BAFTA, you arcane fraternity of troglodytes.
Health
Where medicine meets dignity: Be Well Medical Group founder Isaac Berlin is here and queer to serve the community
A candid conversation with Isaac Berlin on redefining safety and dignity in modern queer-centered healthcare

In a healthcare hellscape that for many LGBTQ+ patients still feels like a labyrinth of pseudo-sympathies, side-eyes, and exhausting explanations, Isaac Berlin is creating something simple yet game-changing. As the founder of Be Well Medical Group, Berlin has made it his goal to ensure that “safe and affirming” isn’t just a catchphrase for PR but an actual experience where patients are met with evidence-based care and genuine respect in equal measure. In his hands, safety is structured, intentional, and protective of both your well-being and your autonomy.
As a clinician, Berlin speaks about healthcare with the clarity and conviction of someone who has seen what happens when medicine fails to listen. From expanding telehealth access across state lines to imagining a future where queer-centered preventive care is the norm rather than the niche, his work is grounded in the core belief that folks do better when they feel safe and heard. In this conversation, we get into what that safety actually looks like, why it matters now more than ever, and how Be Well is modestly reshaping what modern, inclusive medicine can be.
Be Well Medical Group refers to itself as a ‘safe and affirming space for everyone. How do you define what “safe” looks like, and in what ways do you see this evolving in the next year?
At Be Well Medical Group, “safe” care has two essential components: clinical safety and psychological safety.
First, clinical safety means taking patients seriously and doing the work to understand the true cause of their symptoms. Too often in healthcare, concerns are attributed to lifestyle, stress, or personal choices without first ruling out underlying medical conditions. We prioritize thorough evaluation, evidence-based medicine, and avoiding assumptions so patients receive accurate diagnoses and appropriate treatment.
Second, safety means respect for each person’s autonomy and identity. This includes using a patient’s name and pronouns, honoring their goals for health, and recognizing that patients have the right to make informed decisions about their bodies and treatments. We practice shared decision-making, so care plans reflect the patient’s values, not just the provider’s preferences.
Over the next year, safety will also mean greater access. We plan to expand clinic hours and, as demand grows, add additional staff and providers so patients can receive timely care without long waits. We are also continuing to strengthen telehealth options, privacy protections, and trauma-informed communication. Our goal is for every patient — regardless of background — to feel heard, respected, and medically well cared for from their first interaction with us.
You have created a facility where queer folks don’t have to explain themselves to death prior to being cared for. Can you share with us one story that reminds you why you started Be Well?
One experience that has stuck with me was when I was caring for a transgender man with severe vaginal bleeding who was terrified not only of the medical emergency but of how he would be treated. I focused on minimizing trauma and appropriate staff delegation, selection, and education — using the correct name and pronouns, terms, explaining each step, providing medication for anxiety, and ensuring a respectful and thorough handoff when care was transferred.
That experience reinforced why I started Be Well Medical Group: no one should have to choose between getting necessary medical care and feeling safe or respected. While this involved a transgender patient, the principle applies to everyone — patients do better when they feel heard, understood, and treated with dignity.
Telehealth swelled during the pandemic. Do you feel that it has improved access for queer patients or created new obstacles that have yet to be addressed?
Overall, telehealth has dramatically improved access to care. It allows Be Well Medical Group — and the healthcare system more broadly — to bring inclusive, affirming care to patients who may not have it locally, especially in rural or underserved areas. Before 2020, I had patients driving five or more hours just to receive appropriate care. Now I can see patients from places as far apart as Fresno to rural Alaska without them having to leave their communities.
That said, telehealth isn’t a complete solution. Reliable internet access, privacy at home, and state licensing rules can still limit who benefits. But for many patients — particularly those who have struggled to find respectful care — it has been transformative.
If you could create one new queer-centric health screening or service for the 2026 clinic of the future, what would it aim to address?
I would prioritize a comprehensive anal cancer prevention program, including routine screening for anal precancer in people at higher risk. Anal cancer is largely caused by HPV — the same virus that causes cervical cancer — and it disproportionately affects people living with HIV, men who have sex with men, transgender women, sex workers, people with multiple partners, and anyone with a history of abnormal Pap tests or precancerous changes of the cervix, vulva, or vagina.
A modern clinic should offer simple screening tests, HPV vaccination, access to specialized follow-up care when needed, and trauma-informed counseling in one coordinated program. The goal is to detect and treat precancerous changes early, before cancer develops.
While this issue affects many queer patients, it’s ultimately about preventive medicine for anyone at increased risk. Healthcare should focus not just on treating disease, but on identifying conditions that are common, preventable, and too often overlooked.
What issues or concerns are you seeing in Gen Z at the moment, and how are they being addressed?
A lot of what I’m seeing in Gen Z comes down to financial stress, difficulty accessing affordable care, and uncertainty about the future. Many are struggling to get established — whether that’s stable housing, employment, or insurance coverage — which directly impacts their health. There’s also significant anxiety related to the environment, the economy, and a general sense of instability.
Addressing this requires making care more accessible and practical: telehealth, transparent pricing, integrated mental health support, and a collaborative approach that meets patients where they are. When barriers are reduced, most Gen Z patients are highly motivated to take care of their health.
Be Well is community-driven and personal. What are some perks and pains of remaining independent moving forward?
The biggest advantage of remaining independent is flexibility. We control our schedule, appointment length, and care model, which allows us to spend more time with patients who need it and offer more personalized follow-up.
The challenges are mostly structural. Insurance reimbursement for small independent practices is often significantly lower than for large health systems, and the administrative burden to get paid can be substantial. Smaller, clinician-led groups also don’t have the negotiating power of large organizations, which can limit access despite strong community demand.
From your experience, what do you think Be Well offers that those institutions are not able to do despite ample funding?
Personalized care and continuity. In a smaller practice, we truly get to know our patients — their history, what has or hasn’t worked for them, and what matters most in their lives. That allows care to be tailored, not standardized.
Large institutions provide important services, but their size can make relationships feel fragmented. At Be Well Medical Group, patients aren’t just a chart or appointment slot — they’re individuals with evolving needs, and we’re able to follow them over time with consistency and context.
A young queer patient comes into your clinic and says that they left a larger provider after being made to feel unseen. What might be the first thing they notice that tells them they’ve entered a different kind of space?
It actually starts before they ever walk through the door. Our intake process acknowledges that some patients have had difficult or dismissive experiences in healthcare, and we invite them to share what would help them feel safe and respected this time.
Once they arrive, the difference is often in the small details — being greeted respectfully, hearing their name used correctly, and not having to explain or justify who they are. The goal is to create an environment where patients feel understood from the start, not like they have to earn that understanding.
If you had the opportunity to sit down with federal health policymakers for fifteen minutes, what would you ask them to prioritize for queer healthcare in the next few years?
I would urge them to focus on preserving both access to care and the workforce that delivers it. Policies that limit educational funding (recent federal loan caps) for healthcare training risk shrinking the pipeline of clinicians, particularly those from diverse or non-wealthy backgrounds who are often most committed to underserved communities.
I would also emphasize the importance of protecting access to evidence-based gender-affirming care. Restrictions on this care — especially for young people — can have serious health consequences and create barriers for patients who are already vulnerable.
Ultimately, improving queer health outcomes requires ensuring that qualified providers can enter the field and that patients can access medically appropriate care without unnecessary obstacles.
Manning a queer-centric health clinic is likely no easy task. On the more trying days, what keeps you motivated and remaining present for your patients and team?
Healthcare is challenging, and at times, the system can make clinicians feel powerless. What keeps me grounded is the impact we’re able to have on individual lives. Helping someone navigate a frightening diagnosis, reducing their pain or anxiety, or giving them the support to live the life they want makes the difficult days worthwhile.
I’ve worked in healthcare since 2012, and I see my role as both a resource and an advocate for my patients. Even small moments of relief or reassurance can be transformative, and that’s what keeps me showing up.
What’s one thing folks may not realize about what it takes to keep a smaller medical practice thriving in a very corporate healthcare era?
Many people don’t realize that small outpatient practices are typically reimbursed only for actual appointments. Unlike large health systems that may receive broader funding through complex payment arrangements, independent practices rely on scheduled visits to sustain operations. That means even “quick medical questions” or forms require dedicated time.
The upside is that this structure supports more thoughtful care. When patients come in, they receive focused attention rather than rushed responses squeezed between competing demands. It allows us to fully address concerns instead of offering quick, incomplete answers.
Looking ahead to 2026, what emerging health or wellness trend should the queer community be paying attention to, perhaps one that might not be trending on TikTok yet?
One important shift is the growing focus on preventive medicine. Many people assume that needing medication means they’re sick, but in primary care, much of what we prescribe is designed to prevent serious problems before they happen — including heart attack, stroke, kidney failure, heart failure, or blindness.
Modern medicine has dramatically extended both lifespan and quality of life, and prevention is a major reason why. Taking steps early — whether through medication, screening, or lifestyle changes — isn’t a sign of poor health; it’s a way of protecting it.
For more information, head to BeWellMedicalGroup.org
Commentary
Post-Valentine’s Day: Are your standards protecting you — or keeping you single?
As a matchmaker working with LGBTQ folks across the country, I see one pattern over and over again: we are dating with clipboards.
Valentine’s Day has a funny way of magnifying things.
Maybe you promised yourself this would be the year you’d really try: more dates, more effort, more vulnerability. Maybe you did. Maybe you went on five, ten, or fifteen dates. Maybe you tried so hard you’re exhausted.
And yet… here you are. Still single.
Or maybe you’re sitting with a different regret, that you didn’t put yourself out there enough. That you swiped half-heartedly. That you canceled that second date because something felt “off.” That you let another potential connection slip through your fingers.
As a matchmaker working with LGBTQ folks across the country, I see one pattern over and over again: we are dating with clipboards.
We treat dates like job interviews.
We’re evaluating resumes.
We’re checking boxes.
Does he make enough money?
Is he educated?
Does he travel?
Is he top, bottom, or vers?
Is he emotionally available?
Does he want marriage? Kids? A house?
Is he tall enough? Attractive enough? Ambitious enough?
And if he checks every box? Great we’ll proceed.
But what if the real connection isn’t on the checklist?
The Checkbox Trap
Somewhere along the way, many of us decided that compatibility means alignment in every category. We want someone who mirrors our hobbies, our career trajectory, our lifestyle, and even our sexual preferences permanently.
But here’s what I hear constantly from clients:
“I was a top for years. Then I was vers. Then I preferred bottoming.”
“We opened things up later.”
“My priorities changed.”
We evolve. Our sexuality evolves. Our careers evolve. Our emotional needs evolve.
Yet we treat these things as fixed deal breakers before we’ve even allowed chemistry to breathe.
Sexual compatibility matters. Emotional availability matters. Shared values matter.
But are we confusing preferences with prerequisites?
How Many Deal Breakers Do You Need?
By the time many men reach their late 30s, 40s, or 50s, the list has grown long. Very long.
No actors.
No entertainment industry.
No one who earns less.
No one who earns more.
Must want monogamy forever.
Must want children.
Must not want children.
Must be “settled.”
Must be “ambitious.”
Must be hot.
And then we wonder why we’re still single.
I’m not saying abandon standards. I’m asking: are your standards protecting you from incompatibility or protecting you from vulnerability?
Sometimes the truth is harder. Sometimes we seek a partner who feels “worthy” enough so we can feel worthy by association. If I’m with someone impressive, then I must be impressive. If I’m with someone accomplished, then I must be accomplished.
But real intimacy requires something else entirely: self-worth.
When you feel worthy within yourself, you don’t need your partner to prove it for you.
The Twin Flame Mirror
There’s a concept people love to talk about: twin flames.
Whether or not you believe in the term, the idea is powerful. A person who mirrors you. Reflects your strengths and your flaws. Someone who activates you deeply.
What most people don’t realize is that mirrors aren’t always comfortable.
That person who feels “too emotional,” “too guarded,” “too intense,” sometimes they are reflecting parts of you that you’ve worked hard to avoid.
The chemistry may be electric. The connection may take time to unfold. But if you dismiss someone after one date because they showed a crack in their armor, you might be rejecting a growth opportunity.
One date is rarely enough.
People are nervous. Guarded. Performing. It often takes two or three dates before someone relaxes into who they really are.
Attraction vs. Alignment
Yes, you should feel attraction.
But attraction grows.
I’ve watched clients pass on kind, emotionally available, stable men because the spark wasn’t immediate, only to later chase someone wildly charismatic and completely unavailable.
The butterflies you crave? Sometimes they’re anxiety.
The quiet steadiness you overlook? Sometimes that’s security.
If you want the life of the party, ask yourself: are you willing to walk into the party and introduce yourself? Or do you actually need someone slightly more grounded? Maybe an ambivert instead of an extrovert. Maybe someone who lights up in intimate settings rather than on stage.
Compatibility isn’t about sameness. It’s about complementary energy.
Letting Go
After Valentine’s Day, a lot of men insist they’re fine being single. And yes, you can have a full, beautiful life alone.
But let’s be honest. Holidays can sting.
That quiet moment when everyone else seems partnered up. That subtle ache. It’s real.
So instead of doubling down on stricter standards this year, what if you softened?
Letting go. Letting go. Letting go.
What if you stopped asking, “Why won’t this work?” and started asking, “Why could this work?”
What if you looked for green flags instead of scanning for red ones?
Rethinking Monogamy (Without Throwing It Away)
Let’s talk about the word that sends everyone into debate: monogamy.
I believe in monogamy. I’ve seen it thrive. I’ve seen beautiful long-term partnerships built on it.
But monogamy is not declared- it’s developed.
It’s built. It’s earned. It grows from connection.
You don’t have to decide on the first or second date that you’re committing to sexual exclusivity for the rest of your life. And you don’t have to dismiss someone because they’re open to a conversation about what commitment might look like over time.
I’m not saying abandon your values.
I’m saying don’t brush someone off because their view of relationships isn’t identical to yours on day one.
Connection leads. Structure follows.
So Here’s the Question
How many more people do you need to cycle through before you allow one to stay?
How many more perfectly “qualified” bachelors do you need to interview before you realize you’re searching for a feeling, not a résumé?
This year, try something radical:
Give the second date.
Give the third.
Let attraction build.
Let flaws exist.
Let yourself be imperfect too.
Because the goal isn’t to find someone who checks every box.
The goal is to find someone who makes you smile in the middle of a sentence for no reason at all.
And if you can feel that?
That’s not on a checklist.
That’s connection.
If you are ready for a connection join my gaytabase and let’s see who I can connect you with-
Join the Los Angeles Blade, Daniel Cooley, and AJ Socal for our second, free, gay singles mixer at the Abbey this Thursday at 7 pm. It is a low-key and fun way to meet other singles.
Daniel Cooley is a gay matchmaker & co-owner of Best Man Matchmaking – California’s premier service for queer and trans men seeking emotional connections. Learn more here.
Viewpoint
Gay acceptance in US takes a dangerous reversal
Last five years should be wake up call for movement

Shocking news has arrived. New social research says it’s true. Gay, lesbian, gender fluid people, and their allies: we have a problem.
New bias attitude research published by respected social scientists Tessa E.S. Charlesworth and Eli J. Finkel of Northwestern University, based on a longitudinal research program, has shown that gay acceptance in the U.S., which reached its peak about 2020, has taken a deep nosedive in the opposite direction during the last five years. The researchers exclaimed, “This reversal stunned us” — as it did me.
What makes this reversal even more remarkable, as the two social scientists explained, “Americans’ bias against gay people declined faster than any other bias ever tracked in social surveys.” It appears that a new cycle of hetero supremacy has arrived. More likely, the hetero supremacists never went away — just stewing revengefully out of sight around the corner with their buddies from white supremacy and male supremacy.
Analysis of 2.5 million American responses from the beginning of 2021 through 2024 revealed that progress had been turned around. In just four years, anti-gay bias had risen by 10 percent. Researchers followed both explicit bias (to what extent do you prefer straight people over gay people?) and implicit bias (more automatic responses inferred by how rapidly people associate words, such as straight with “good” and gay with “bad.”)
Most disturbing of all, these trends were particularly strong among the youngest American demographic, those under 25, a society’s hopes for the future. Also noteworthy was that anti-gay bias has grown faster among conservatives, but it had also risen among liberals.
The researchers admit they have no idea what is causing this dramatic reversal. They suggest two possible hypotheses: (1) anti-trans bias and (2) fear of gays grooming children to become gay, an essential part of hetero supremacists’ baggage of hate for the past 125 years in the West. Children cannot be groomed into being gay but are born that way for an evolutionary reason (more on that subject in a later article.)
Let me add a third hypothesis based on my close, active involvement and observation as a gay community organizer over the past 60 years. A big part of the problem is gay people themselves. If you have followed my many writings over the past 25 years, you have heard this sermon several times before in varying language and contexts.
The Gay Liberation Revolution (1969-c.1985) taught gay and lesbian people that gay peoples’ self-acceptance and united action are more powerful than hetero supremacy. A Gay Liberation tidal wave provided the momentum for a “movement” forward for our people. Now, that tsunami has become a ripple. How did that happen?
1. The absence of a gay political movement. A political movement is “an organized effort to promote or obtain an end.” There are people who I respect who delusionally speak as if a gay movement still existed. A Gay Liberation template does exist for what a gay movement might look like. It must be played forward, however, with the language, reality and tools of today. It begins with the question: How am I and my community oppressed today by hetero supremacy? Action grows out of oppression.
2. The dominant ideology of gay assimilation. As James Baldwin preached, assimilation is always done on the terms of the dominant culture. For gay people, assimilation implies the eradication of hard-fought-for community and identity. Gay and lesbian people, where did you disappear to? Just yesterday, you were here with your fists in the air.
3. Elite capture of the gay community. This capture is characterized by a top-down power structure (elite vertical axis), community members (grassroots horizontal axis) becoming passive spectators, and the primary priorities being wealth, donors, and celebrities, not community well-being. The call for gay power devolved into donate and consume.
4. Community fragmentation by visual media. The dark side of the current new tech visual media avalanche is the fragmentation of a formerly good-enough-united gay community. Visual media has turned community awareness from “we” to “me.” Local news and investigative journalism have disappeared completely from gay news sites that are now “curated.” A good example was the implosion of Outfest: the LGBTQ Film Festival in L.A., a major community cultural institution for half a century. Gay people found out about that truly shocking community news after Outfest’s disappearance by an investigative journalist at the Hollywood Reporter;the financial malfeasance of GLAAD was uncovered by the New York Times, not gay news sites. Without investigative journalism, community members do not have the information spotlight that is essential for being actively involved and engaged in a healthy community.
5. Pick off the low hanging fruit first. I often hear from others that trans people have taken over the movement. My standard reply: “Because gay and lesbian people have voluntarily disappeared from their political movement, a vacuum has occurred. Vacuums are always filled by something. Trans people are not the problem. There is a problem: your disappearance. The main problem, however, and never forget this, is hetero supremacy.” The hetero supremacists’ playbook is the same used to rescind Roe. Get the low hanging fruit first — under 18 trans youth. Then, proceed calculated step-by-step to the main target — YOU AND ME. Supreme Court Justices Alito and Thomas maladroitly revealed their goals: (1) rescind gay marriage and (2) recriminalize same-sex sexual acts.
A dark night of the gay community’s body and soul might be coalescing. As with all such dark nights, a new sun will rise with renewed vigor and vision, with gay righteous mind and mindfulness replacing today’s mindless scrolling, streaming and surrendering. As the old United Negro College Fund wisely said, “A mind is a terrible thing to waste.”
Don Kilhefner, Ph.D., is a pioneer gay liberationist and a gay community organizer in Los Angeles, nationally and internationally for the past 60 years.
Commentary
Valentine’s Day, Alone
We the People are embracing and uplifting our own and each other’s humanity.

Valentine’s Day. Permission to briefly set aside mental acrobatics and just feel. Over the years, I’ve gone from Elvis’ “Can’t Help Falling in Love” to the lesbian version of Beyonce’s “Single Ladies.” And after we won marriage equality, I shed happy tears to “Same Love” by Macklemore & Ryan Lewis and Mary Lambert, even though I was alone.
The truth is, my longest relationship lasted five years. I don’t need therapy to tell me it’s my fault. I always secretly hoped that each woman would rekindle the flames of my first love. Yes, she was straight, and it was incredibly complicated – but it was also the Age of Aquarius, and for this budding Aquarian hippy-wannabe, it was mythologically perfect, as doomed as I subconsciously knew it was.
So, Valentine’s Day always had a slight shade of pain.
But I had my dogs. I didn’t need romance – I needed love. And over the years, what happy times we had, watching some action movie and sharing the crust of a great Hawaiian pizza.

I thought this Valentine’s Day would be the same. Actually, Pepper, my 18-year-old Cairn Terrier, has been my longest relationship of all. I rescued her when she was five. She was living in a Latino family, beloved by a young teenage boy who called her Sparky. But one of their two other dogs didn’t like her, so they had to give her up for her own safety.
The boy tried so hard not to cry when they dropped her off – but Sparky wailed and wailed. My neighbors looked out to see what was wrong. I did what I could to ease her sense of abandonment. I even learned a little Spanish and changed her name so she wouldn’t be retraumatized every time I called for her. My other poodle-ish dog, Charlie, and I had to wait for her to trust us.
In time, Pepper and Charlie bonded. When he got sick, I took her to hang out with him in the hospital, bringing her home at night. Charlie died of a seizure overnight without us.
Not long after, my friend Gloria Nieto called to see if I would be interested in adopting this little boy dog who needed a new home asap. Gloria lived in the Santa Cruz area, so we decided to meet halfway in San Luis Obispo to see if the two dogs got along. They did, Papa D came home with us, and I became friends with Papa D’s heartbroken mom on Facebook.

Pepper and renamed DeeJ bonded quickly, with Pepper becoming something of a mother. One time, I was surreptitiously watching them play at a wonderful doggie day care on Ventura Boulevard. The attendant wasn’t in the room when a bigger dog started menacing DeeJ, who backed into a corner, shaking. Pepper went and sat next to DeeJ, but when the bigger dog didn’t back off, Pepper, who was also scared, got on her belly like a supplicant and crawled between the bigger dog and DeeJ. I ran back inside to get them and take them home to West Hollywood.
I’ve never forgotten Pepper’s incredible bravery, inspired by love. When DeeJ died, we were both bereft. At times, we would independently hear a sound like a bowl being moved in the kitchen and look up, expecting DeeJ to come out and bound across the floor at any moment. Then we’d hug.
After a while, I adopted Keely, who was deaf. Keely wasn’t interested in bonding with Pepper. But she wasn’t with us very long – she had a massive cancerous tumor, and the prognosis for survival after surgery wasn’t good with her other ailments.
After Keely died, I decided Pepper would be the only dog. The two of us, alone. And despite having Cushings, having to undergo surgery for a small tumor, developing kidney disease, and starting the beginning stages of doggie dementia, Pepper was doing incredibly well.

And she was incredibly sensitive to my moods. On Wednesday, Feb. 11, after we’d come home from her grooming, I tuned into ice dancing at the Olympics. The Canadian couple skated so beautifully to “Starry, Starry Night,” tears started streaming down my face. Pepper bolted up, looking at me quizzically but with doggie empathy before coming over to lick my tears and give me kisses. She eased slowly across my chest to hug me.
The song stuck with me, looking at the waning crescent moon as we went on our brief nightly walk. In the carport before we came home, we ran into our neighbor and her young Shih Tzu from the building next door when another neighbor and his big dog came down the alley. Suddenly – in a flash – the big dog jumped up, tearing off his leash, and lunged towards the Shih Tzu. Seconds later, she jumped onto Pepper.
We all freaked. I was knocked down in the struggle to free Pepper. By the time I got to her, she was listless and bleeding – but still had a pulse. Another neighbor madly dashed us to the Emergency vet as I told Pepper how much I loved her and to please stay with me. But she couldn’t. She died in my arms.
I was devastated but not freaked out – I’ve held dying friends and dying dog/kids before. But the sudden violence I was powerless to prevent made this different. My apartment was suddenly big and empty and quiet – even with TV politics in the background. Images of Pepper’s bloody body lying on the concrete blinded me. I blurted out her name and reached for where just hours earlier she snored softly, her skinny, aging body snuggling next to mine. I changed channels, looking for something comfortably mind-numbing. Unbelievably, I came upon a replay of the Olympics and “Starry, Starry Night.”
After a sleepless night, I had a 12 Step phone call with a friend who lost her precious cat last May. She suggested that this first stage of denial was akin to the deep, difficult First Step of surrendering. That made sense to my journalist/observer side, who advised my jumbled emotional side to be patient and, as 12 Steppers say, “feel the feelings” when they come.
This June, I’ll be 46 years clean and sober. But I now feel like a newcomer again. That’s good because it gives me permission to be weak, to acknowledge that I need help, and accept the love that’s being so generously offered.
And here’s where this tragedy becomes extraordinary.
Early next morning, my 12 Step neighbor – who’s 88, BTW! – knocked on my door. She brought a bag of food from someone from the building next door, who was among the slew of neighbors who rushed out, hearing our anguished cries. She said it felt like community – even though we only knew each other through our dogs. I was Pepper’s mom.

And this made me hesitant to report what happened. As I struggled to get up and get to Pepper, I saw the father of this big dog hold him tightly and break down. “I can’t lose another one,” he cried over and over to his wife. Apparently, he just lost his father. We all didn’t need a second tragedy. But Pepper’s death was a preventable fatal accident, and he still had to be accountable.
I struggled with this. Knowing him as a dog-loving neighbor, I suspected he and his family were devastated. So, I forgave him and the big dog, who was so sweet on the street. I then called several neighbors, thanking them and asking for advice. One neighbor felt it was important to report because this dog had bitten two other dogs over the years, and what if this dog attacked a person? Another neighbor understood my dilemma and offered to back me up, no matter what, but said she no longer felt safe in the community.
And there it was. Yes, my feelings mattered – probably tied to my guilt at not being able to protect Pepper, as this man was trying to protect his dog/child from certain execution. But community mattered more.
Then the big dog’s mother called, totally devastated and deeply apologetic. They have two young daughters whom they’re trying to teach about doing “the right thing,” so they had already called Animal Control to report what happened and find out what to do next. I told her that I forgave them – but they had to be mindful of community safety. I also asked her to please teach their children that not every bad event demands rage and retaliation in response. Love and understanding are really important right now.
She cried and called back later to say they had decided to put their beloved big dog down themselves so they could say goodbye as a family. Our community has responded with empathy and support for them now, too.
So, while I continue to struggle with feeling my feelings and realize that this Valentine’s Day, I really am alone, I also feel surrounded by love, including from my MAGA friends, and thinking of DeeJ and Pepper reunited.

There is something going on. Not just here, in our little corner of West Hollywood embracing tragedy and forgiveness; or in anti-ICE protests remembering Renee Good and Alex Pretti; or the almost universal outpouring of love and joy in Bad Bunny’s Super Bowl halftime concert.
We the People are embracing and uplifting our own and each other’s humanity.
Sing it with me: “What the world needs now is love, sweet love. It’s the only thing that there’s just too little of.”
Happy new post-Valentine’s Day!
This essay is updated/cross-posted from longtime LGBTQ+ journalist Karen Ocamb’s Substack LGBTQ+ Freedom Fighters.
Commentary
What Grindr’s pricey new subscription says about the gays, intimacy, and capitalism in the age of AI
Grindr’s shiny new Edge subscription epitomizes how dating and hook-up apps monetize loneliness by selling algorithmic control as a substitute for genuine human connection

This February, Grindr discreetly started testing out a brand new premium subscription tier, Edge (props on the wordplay), powered by its proprietary generative AI stack appropriately named “gAI™.” The catch is that some users are being asked to pay more or less the price of one hour of an escort’s time for one month’s subscription. This would place Grindr’s top tier soaring above most mainstream dating apps (Tinder, Hinge, Bumble, etc.) with prices higher than Nicki Minaj on a MAGA stage, some can’t help but wonder who the target consumer is.
At face(less) value, this feels like a corporate strategy to squeeze more money out of a perhaps struggling “dating” app. Grindr’s stock has gone limp, and it’s pushing AI as the ED med that will fluff it up into a smarter, faster, more personalized user experience. But when you really look at it, this pricing experiment speaks volumes about the current state of our gay community, intimacy, desire, and the toxic top that is capitalism in the age of artificial intelligence.
Grindr entered the scene (and the app store) in 2009 as a simple and sweet grid of nearby dudes scoping out who’s around and down to get down. It was immediate. It was raw. And, perhaps most uniquely, it was physically grounded. But like most apps and platforms do over time, features were paywalled, and basic functions became privileges. The free portion of the grid shriveled like a pair in winter air. Ads multiplied and became more aggressive, like a digital strain of super gonorrhea. Want more? Pay. Want to be seen? Pay. The death grip of capitalism knows no lube.
This transformation is a testament to a larger pattern in tech called enshittification (aka crapification), where platforms become increasingly more hostile to their users as their money-goggles fog up with greed. Grindr’s Edge is the latest example; a subscription promising personalized AI-generated matches and chat insights, all with the promise of more “meaningful connections.” With price hikes reaching close to half a grand, one can’t help but wonder what is actually being commodified here.
Gay lust is no stranger to consumer culture. From marketing fitness (“Look Better Naked”) to gay-centric grooming (shoutout to Good Head, we see you king), sex drive and commerce have been bedfellows longer than the grandparents from Willy Wonka. Hook-up and dating apps, simply put, commodify attention. Profiles are products. Swipes are currency. Desirability is now quantifiable, folks. Take this concept, feed it one too many bumps, and you’ve got Edge.
What’s happening, my fellow homosexuals, is the premiumization of intimacy. Not just matchmaking, but the promise that technology can deliver connection… for the right price. And the price of this new tier of service says more about our collective culture at this moment than it does about the greedy little piggies behind Grindr. We live in an age where AI is infringing on emotional territory once thought to be uniquely human. Algorithms already curate our newsfeeds, recommendations, and shopping lists. And now, well, we can tag “digitally omnipotent yenta” to the tally.
The creation of Edge also highlights how modern capitalism treats desire as an inefficiency that can be solved. Grindr is utilizing a not-so-new strategy here: hone in on its users’ loneliness and fear of rejection and redesign features that address these feelings… at a premium. One undeniable takeaway is that genuine interactions are no longer occurring naturally.
On a psychological level, Grindr’s Edge subscription tugs at the arguably universal hunger for control. In a world brimming with flirtations that flatline, DMs that die down, and dates that don’t pan out, the allure of AI as a fail-safe is, well, seductive. But what happens when that illusion of control clashes with the actual intimacy that we seek? Instead of enhancing connection, AI could fossilize it, making real human interactions that much more transactional than said apps have already made them out to be.
Grindr’s Edge experiment reveals how capitalism monetizes the desire for human connection, how tech sells the guarantee of ease void of authenticity, and how intimacy in the digital age increasingly becomes a slave to the algorithm. Yet resistance is already clapping back. Online discourse from users dragging Grindr for the high prices and migrating to alternative platforms shows us that many are not buying into the premiumized dream.
Ultimately, Edge feels less like an innovation and more like an admission: that instead of fostering environments where vulnerability and spontaneity thrive, platforms would rather engineer a shortcut and charge stratified admission. When the illusion of confidence is packaged as a purchasable upgrade, the entire thing starts to feel that much more bleak. Stripped of its shiny branding, it reeks of incel-scented desperation, a tech-mediated fantasy that mistakes control for chemistry and convenience for closeness.
I may stand alone in this humble opinion, but a dude who’s audacious (or foolish) enough to sign up for such a service is a hard pass. In the end, shop local – hire an escort. At least then nobody is denying the pure transaction of it all.
Commentary
Are we done with ‘Drag Race?’
While the show may feel a bit formulaic, and we long for the days of earlier seasons, where we met luminaries like Alaska, Jinkx Monsoon, and Bob the Drag Queen, the larger question is whether the show is more focused on straight audiences.

RuPaul’s Drag Race has left an indelible mark on history. What started as the bastard love child of America’s Next Top Model, Real Housewives, and Project Runway has birthed an entire industry of drag race content, from tours to review podcasts. It’s elevated its stars to international stardom and reshaped the queer economy with its impact on bar culture, marketing to queer people, and Mama Ru pushing her girls to sell.
While conservatives have declared war on drag, the show has held strong. Now in its latest and 18th season, a show that has united the whole LGBTQ community in inside jokes and pop culture references has offered the community its own sports equivalent and instant “in” to a conversation.
The question arises: Are we done with Drag Race?
Considering how Heated Rivalry became a ratings behemoth despite being an independent Canadian drama, and viewers seem more galvanized about the queer representation on The Traitors, have we developed Drag Race fatigue? The show hit a high point with franchises in countless countries, with RuPaul even crossing the pond for the UK and the earlier versions of the Australian series. The political and economic fuckery of our current state of affairs has even hit Drag Race.
While the show may feel a bit formulaic and we long for the days of earlier seasons, where we met luminaries like Alaska, Jinkx Monsoon, and Bob the Drag Queen, the larger question is whether the show is more focused on straight audiences. In a post-Trixie & Katya world, it seems there’s a choice in the world of drag: are you courting queer or cis-het audiences? Do you become gay famous and never pay for a drink again, or do you pander to straight women and make bank?
The issue may not be that Drag Race as a show has become the problem, but it’s just become too normative. How could a show with new queens each year feel…less than fresh?
The show seems to have drawn a line in the sand by defining what is “good drag,” so you end up with a cast that could be anyone with a Sephora gift card, OCD, and a budget for lavish costumes. The latest season broke from its recent trend of casting young, social media-savvy queens opting for more seasoned performers in their 30s and 40s. They’re then labeled as old. “Be still, my heart!”
Part of what drove the show and the major cultural movements was queens being themselves and finding artistic solutions to their shortcomings. But we’ve reached ouroboros with queens communicating entirely in Drag Race references. The contestants are self-producing and trying to force storylines, catchphrases to sell merch, and court a yet-to-be-determined audience to try to make back the money they invested or try to stay relevant in a pool of girls that’s reached three digits.
The show is becoming a bit too self-aware. The challenges are a bit repetitive, and seasons of Drag Race are starting to feel a bit like a Law & Order episode. By episode 4 or 5, you can peg who is the winner, who is the delusional starlet whose ego RuPaul must crush to claim 7 more years of youth (hi, Jan!), and who is the villain.
The predictability betrays what’s behind the curtain. There’s a bit of manipulation to venerate queens who have the savvy to carry the brand. But is it at the cost of some of the show’s integrity? For example, this season, it was clear Mandy Mango was not on par with the other girls with regard to styling and make-up, but having the judges tell us that she wasn’t funny in her sketch or that she didn’t win a lip sync feels a bit too far. In an era of “fake news” and media manipulation, can you trust a show that tries to tell you the sky is not blue but fierce?
In an earlier season, a personality like Mandy’s might have won, a la Jinkx Monsoon. There is also all that we don’t see, given a notoriously toxic fandom, the show runs the risk of activating a fanbase primed with racist torches and pitchforks.
It’s an open secret that RuPaul’s Drag Race is more of a reality show than a competition, but that might be impacting its longevity. With Tyra Banks facing a documentary covering some of her insane stunts on America’s Next Top Model while Project Runway is still alive and kicking, it’s clear that if Drag Race wants longevity, it needs to value its integrity.
After all, in an alternate timeline where Drag Race was honoring its LogoTV roots, it might have featured Connor Storrie and Hudson Williams as guest judges or tapped Alexander Skarsgard from Pillion rather than female celebrities who offer the A or B-list equivalent of bachelorettes at drag brunch like the now-canceled Nikki Minaj and Whitney Cummings.
As we careen closer to an autocracy, do we deserve a reality show that keeps it real? We have reached a point where what we have allowed to continue has come to bite us. Choosing capitalism over integrity is a tacit support for corruption. In a time where the queer experience is fundamentally unfair, should we have a reality comparison that’s inherently unfair?
All this being said, Drag Race is still doing its part to support the bar industry. Some viewers have found it hard to watch Drag Race without purchasing episodes, potentially because its ties to CBS/Paramount/MTV World of Wonder are still creating content for the community.
Canada’s Drag Race still takes chances and casts a diverse group of queens, and it seems like a fairer contest. Surviving a revolving door of hosts, the show has managed to stay fresh and engaging. Drag Race UK also has retained a lot of the interqueen chemistry that drives the show with drag queens who know how to read, kiki, and maintain good working relationships rather than pandering to television drama.
Drag Race is essentially sports for people who don’t like sports. Drag Race gives us our own arena where our queers can highlight aesthetics, drama, stunts, and humor. We all make our draft picks during the Meet the Queens premiere, and we wear merch for our favorite players. But if the show divests from queer culture to make a buck, you end up with straight women criticizing the work of multiple artists and tens of thousands of dollars of effort because they don’t like someone’s aesthetics or they have “bad make-up.”
The show started as a platform for a forgotten but timeless art of queer people dressing up as women to lampoon toxic masculinity and internalized homophobia while serving as den mothers, brassy broads, and queens of our community to help make being gay a little more fun, flirty, and cunty.
I hold out hope for Drag Race, but I do think it would serve them to be a bit more beholden to the queens they cast, the community they serve, and focus on the contest itself rather than choosing fairweather political allies and lookie-loos and homogenizing drag at the expense of its political punch.
AIDS and HIV
Congresswoman Maxine Waters introduces new resolution for National Black HIV/AIDS Awareness Day
H.Res.1039 supports more funding, resources and awareness for Black American communities, who are disproportionately impacted by HIV/AIDS.

Today is National Black HIV/AIDS Awareness Day. Advocates established this day of awareness on Feb. 7, 1999, and nearly 30 years later, Black communities in the U.S. continue to be disproportionately impacted by HIV.
On Wednesday, California Congresswoman Maxine Waters introduced H.Res.1039, a resolution that supports the goals of National Black HIV/AIDS Awareness Day and calls for a collective commitment to address disparities Black people with HIV face. Waters represents the state’s 43rd congressional district, a majority Black and Brown population comprising South L.A. cities like Hawthorne, Gardena, and Inglewood.
In the resolution, Waters urges state and local government officials, as well as their public health agencies, to acknowledge the importance of this awareness day and encourage their constituents to get tested for HIV. The resolution also requests that the Secretary of Health and Human Services prioritize distributing grant funding to minority-led, HIV organizations and community-based approaches to fighting HIV stigma, LGBTQ+ discrimination, and racism.
In 2023, young Black men accounted for 47% of new HIV diagnoses among youth, while young white men made up 3% of these diagnoses, according to a new Williams Institute report. Black women also have the highest HIV diagnosis rate among women, and Black community members overall represent 38% of new HIV diagnoses and 39% of people living with HIV in the U.S., despite being only 12% of the national population.
Beyond the disproportionate rates of infection and diagnosis amongst Black Americans, these communities also face greater difficulties in accessing the medical care needed to prevent and treat HIV. In the same year, white Americans were 7 times more likely to access Pre-exposure Prophylaxis (PrEP) compared to Black Americans, a data point that affirms racial and healthcare inequities Black people continue to face in the U.S.
“[This] is a day to commemorate the impact of HIV/AIDS on Black Americans and encourage continued efforts to reduce the incidence of HIV, eliminate health disparities, improve access to care and treatment, and show support for all those who are living with HIV/AIDS,” said Congresswoman Waters, in a press release.
Waters has been an advocate for people impacted by HIV/AIDS since the peak of the crisis in the 1980’s. In 1998, she worked to establish the Minority AIDS Initiative, which expanded national prevention and treatment efforts in support of minority communities, who remain disproportionately impacted by HIV. In 2025, Waters introduced the “HIV Prevention Now Act” as well as the “PrEP and PEP are Prevention Act,” to increase prevention efforts and reduce health insurance barriers to access preventative resources, respectively.
H.Res.1039 is the latest addition to the congresswoman’s efforts to raise awareness for Black and other minority communities impacted by HIV/AIDS, and to fund and support on-the-ground efforts that prioritize their care and wellbeing.
The resolution is endorsed by various LGBTQ+ organizations mobilizing for communities impacted by HIV, including AMAAD Institute (Arming Minorities Against Addiction and Disease), LA Pride, AIDS Foundation Chicago, and PFLAG National. The resolution is also co-sponsored by 29 other U.S. representatives, including fellow California congressmembers Robert Garcia, Laura Friedman, Nanette Barragán, Sydney Kamlager-Dove, Lateefah Simon and Mark Takano.
H.Res. 1039 has been referred to the House Committee on Energy and Commerce, and currently awaits further action.
Kristie Song is a California Local News Fellow placed with the Los Angeles Blade. The California Local News Fellowship is a state-funded initiative to support and strengthen local news reporting. Learn more about it at fellowships.journalism.berkeley.edu/cafellows.
The success of Heated Rivalry has brought up an interesting question: is the fact that these two sexy hockey players are fundamentally unavailable the secret to their forming a deeper, meaningful relationship? Is the possibility of intimacy and romance based on the fact that they can’t have it?
Sure, that’s fiction, but after my breakup with an aspiring “poly” Scorpio with an avoidant attachment style, I spent a year being a fuckboy. I thought growing out my beard was a game-changer, but being emotionally unavailable was like having three dicks. Having no interest in a romantic connection somehow made it so much easier to get laid, meet guys, and connect without running the risk of sabotaging things.
I was shocked by how much attention I got. It’s like guys could smell the unavailability, and it fueled me having connections more deeply than when I was available. I’ve always struggled with the idea of playing hard to get. Why would I pretend I don’t like someone? Isn’t that lying?
And yet, it seems like that is the secret of success. I was recently reconnecting with a guy. We had a ton of great chemistry, common interests, and were really excited to get together. He was sick, so we couldn’t hang out. My eagerness to meet may have gotten the best of me because rather than finally meeting, he broke things off, saying he wasn’t ready for anything deeper.
As I switched from being emotionally unavailable to primed to date, I lost all of my emotionally unavailable powers. I even had to ask myself if I had fallen into the same trap. Was I so attracted to him because he was definitely not a love match? Why do we constantly seek out people who are unavailable?
Sometimes, you have the freedom to really let yourself go and put down all your walls because you know subconsciously there are no stakes because the relationship has an expiration date. It reminded me of a conversation I had with a friend.
He had hooked up with someone on a boy’s trip and was lamenting that this guy, who already had a partner, did not have the same feelings. We had a long conversation from NorCal back to Los Angeles reflecting on attachment styles, romance, and our longing for connection.
Then our friend broke all of our brains. He asked if he was addicted to the feeling of longing. That exciting feeling you get from someone new. He pointed out, what if on some level my friend was not just attracted, but dare I say attached, to the feeling of fundamentally getting rejected?
You can’t look at gay relationships and not think of trauma. On some level, the decision to pursue your same sex attraction comes with the potential to be voted off the island. In extreme cases, you get thrown out of your house. Your relationships can change, leaving a rejection wound that we like to pick at every time we date some fuckboy, guy with a partner, or someone who is fundamentally bad for us.
Our community is a bit like the Wild West. You can end up on the wrong side of someone’s unresolved issues with their family, sexual assault trauma, or the bad karma of their past relationships. Gay men are trauma survivors who can traumatize each other.
Our dating pool is also our pool for friends, rivals, business contacts, and romantic partners. And yet, why is it that the people who are unavailable, like cream or scum, rise to the top? Is the allure of the unavailable the retraumatization of our messy familial relationships? Is it revisiting the longing of our queer awakening for that first guy who didn’t choose us? Are we chasing some initial early wanting we developed in the closet?
Are we chasing the fantasy of love and projecting that onto some guy who feels ambivalent to us? It’s worth asking these questions because if we look at our friend groups and dating histories, charting the complex boundaries and intermingling connections is like watching a Ryan Murphy show with better writing.
But it goes deeper. Are we sabotaging relationships by rejecting people who like us? After all, as men, it’s not unheard of to have a bit of a fear around intimacy and vulnerability. There’s also the fundamental scientific and economic concept that scarcity equates to value. So do we chase someone who has a greater premium on their time and attention?
As queer men, we hack our bodies to get in better shape, and many of us do that with our relationships. We end up forming a complex system of fuck buddies, situationships, intimate platonic friends, and crushes, forming a distorted jigsaw puzzle that forms the equivalent of one relationship. Meanwhile, what would it be like exploring what it would be like to just spend time with one person and then putting them back in the pond for someone else?
There are men in open relationships who spend more time in the pursuit of sex and male attention than single folks. There are friends who use their friends’ unresolved sexual or romantic feelings to have their intimacy needs met while playing the field.
This could just be the nature of city-dwelling gays in a city like Los Angeles. After all, to have countless options, guys end up with an ever-growing list for Santa of the man who’s “worth” settling down for.
Can we just appreciate when someone likes us? How can we focus on the positive and support a queer brother who, despite all the political fuckery of our society, still has the confidence to put themselves out there and choose love? Can we reject without crushing someone’s spirit or introducing unnecessary drama?
What if we love ourselves enough to realize we deserve love and the people we’re with to love us back?
Can we not put undue pressure on the men we fancy to not just be the object of our affection but the sum of all of the things we’re not dealing with, the solution to our unreseolved childhood romantic feelings, and fulfilling an ever-evolving fantasy?
At the end of the day, we have to all realize we are all people who have more in common than we have differences, stop projecting our problematic pasts or hopes for the future onto each other, and learn a little bit about how to love better. That way, we can be present with the people we are with rather than cast them in roles in the soap opera in our heads.
-

 Arts & Entertainment3 days ago
Arts & Entertainment3 days ago2026 Best of LGBTQ LA Finalist Voting
-

 Health4 days ago
Health4 days agoWhere medicine meets dignity: Be Well Medical Group founder Isaac Berlin is here and queer to serve the community
-

 Out & About4 days ago
Out & About4 days agoQueer, trans AAPI joy shone at this year’s Golden Dragon Parade
-

 Mexico5 days ago
Mexico5 days agoUS Embassy in Mexico issues shelter in place order for Puerto Vallarta
-

 Commentary3 days ago
Commentary3 days agoWhen optics matter more than harm: BAFTA, BBC, and editing solidarity while letting slurs slide on through
-

 California3 days ago
California3 days agoExperts discuss pathways forward as anti-trans violence continues to rise
-

 Autos4 days ago
Autos4 days agoGoing for gold: Ford Bronco Sport vs. Toyota RAV4
-

 a&e features3 days ago
a&e features3 days agoRevry Co-Founder Damian Pelliccione on why we need ‘King of Drag’
-

 Books3 days ago
Books3 days agoNew book profiles LGBTQ+ Ukrainians, documents war experiences
-
 Books2 days ago
Books2 days agoThe social side of self-pleasure: Artist Jason Wimberly presents his newest book of photography, HOMOSOCIAL










