AIDS and HIV
Raniyah Copeland, Black AIDS Institute’s new leader


“Our house is on fire!” Phill Wilson preaches from the pulpit at Holy Name of Jesus Church in Los Angeles, Newsweek reported June 10, 2001. “AIDS is a fire raging in our community and it’s out of control!”
Wilson founded the Black AIDS Institute two years earlier, in May 1999, to shout “Our house is on fire!” from every pulpit, stage and rooftop he could find as whites with access to the new three-drug cocktail saw HIV/AIDS turned into a manageable disease while new infection rates in the Black community continued to skyrocket. Though not horse from shouting – and having made extraordinary progress in the almost 20 years serving as President and CEO of Black AIDS Institute (BAI)– Wilson announced his retirement in 2015.
After a concerted search, the BAI Board announced a new director on Dec. 1 during their annual Heroes in the Struggle gala: Raniyah Copeland, 34, a BAI executive staffer was picked out of 20 applicants. “I can’t imagine a better choice to lead the institute into the future. Raniyah is bold, brave, and brilliant,” Wilson said about his successor. “She brings a vigor and vision to the AIDS movement that, given the current political environment, is desperately needed.”
And Copeland does “bring it.” Backed by degrees in African American Studies from the University of California/Berkeley and a Master of Public Health from Charles Drew University of Medicine and Science, Copeland started her dream job at BAI combining her two passions—Black people and health—in April of 2008, first as the Training and Capacity Building Coordinator and now as Director of Programs, until Jan. 1 when she assumes the CEO mantle.
“What’s really important to me is Black people,” Copeland tells the Los Angeles Blade when asked why a straight married mother of two would want the job. “It’s really quite horrible that we aren’t all really outraged by what HIV looks like in Black communities. HIV disproportionally impacts same-gender-loving people, trans folks, and Black cis women. I am a cis-hetero-woman—but we are one community and I think that for me, it sends an important message that we are in this together.
“The only way we are really going to end HIV is by our entire community coming together,” Copeland says. “It’s important that we all do our work to end HIV stigma and homophobia and transphobia—and that’s not the work of only some same-gender-loving people. It’s work we all have to do and I’m excited to lead that effort.”
It’s an excitement fueled by the lessons of history. “I was raised by what folks might call two radical Black parents. Growing up, I learned a lot about the history of Black people, the oppression of Black people,” she says. “A monumental book for me was ‘A Taste of Power: A Black Woman’s Story’ by Elaine Brown, who was the highest ranking Black woman in the Black Panther Party. I remember thinking that we as Black people have so much to offer and we’ve been through so much, that it was disgraceful that Black people were disproportionately impacted by so many diseases, whether it was breast cancer, diabetes or HIV.”
In college, Copeland worked on reproductive justice issues but was startled writing a report on HIV in Black communities. “I thought how crazy it was that there was this huge HIV epidemic and the highest amount of attention that I ever remembered was around Magic Johnson,” she says. “But there were all these other communities within the Black community that were disproportionately impacted. It didn’t sit well. It didn’t seem right that HIV wasn’t getting the attention that it deserved—it didn’t seem like people cared very much.”
After college, she was thrilled finding a BAI job posting. “Who I am is being able to be uniquely, unapologetically Black. So finding an organization that focused on that was really exciting for me.” And doing HIV work across the country, “really showed me how the epidemic looks so different in different places.”
Copeland’s work is intersectional. “Mass incarceration is one of many themes that is really so important to ending HIV. We work with Black Lives Matters closely and make sure that HIV is part of the policy agenda and the work that they do,” she says. “For many people, particularly Black people, HIV is not the primary concern. Whether they’re going to get shot by police is a primary concern; whether there’s food on their table is a primary concern; whether they’re able to be in safe relationships free of intimate partner violence is a primary concern.”
So how make HIV important? “Respond to those issues,” she says. “To really respond to HIV, we have to discuss the issues that trans people have: how do we ensure that trans folks are supported? How do we ensure that trans folks have access to quality healthcare that’s culturally humble? And make sure they have opportunities to education and employment?”
Part of the answer is by partnering with different organizations. Which leads to: “how do we provide services that are culturally humble? How do we work with institutions to teach them how to better serve Black communities? These organizations are not HIV-specific but they are critically important working on issues such as employment or legal support or education,” Copeland says. “Those are the services and the relationship and the partnerships that we have to develop and further to ensure that the communities that we serve have the support and resources that are part of being human.”
Copeland is excited about BAI’s new expansion into direct services and partnering with different organizations, such as St. John’s Well Child & Family Center. “We end HIV,” she says, by creating access to quality healthcare that’s “culturally humble” and “by making sure that people have access to the human rights and the dignity that they deserve.”
Being culturally humble, Copeland explains, “is a step above being culturally competent. Cultural competency means you have an understanding of the norms and the culture that people come from. You understand the language that you should and shouldn’t use. You understand medical mistrust that is present in Black communities. You understand the need of trans folks and how they different from cis people. These are all things that you learn. Cultural competency – you understand the culture.
“Being culturally humble means that even though you know you have a competency, that each person is going to present to you differently,” Copeland says. “No culture is monolithic. So when people present to you, you have the competency but you let them guide and you let them determine the kind of services they want. It’s a different type of framework around how you position the relationship. And really understanding that the people we serve, the people that we engage with – that they lead us.”
But 57% of new HIV infections are among 13 to 29-year-old African American youths, according to the CDC, and reaction to using PrEP, Pre-Exposure Prophylaxis—using anti-HIV medications to keep HIV negative people from becoming infected – has been mixed.
“Pre-exposure prophylaxis (or PrEP) is when people at very high risk for HIV take HIV medicines daily to lower their chances of getting infected. PrEP can stop HIV from taking hold and spreading throughout your body. It is highly effective for preventing HIV if used as prescribed, but it is much less effective when not taken consistently,” the CDC reports. “Daily PrEP reduces the risk of getting HIV from sex by more than 90%. Among people who inject drugs, it reduces the risk by more than 70%. Your risk of getting HIV from sex can be even lower if you combine PrEP with condoms and other prevention methods.”
HIV reporter Emily Land writes: “Only seven percent of participants part of a PrEP demonstration project conducted in three major U.S. cities between 2012 and 2013 were black, and one study found that heightened concerns over potential side effects may pose one significant barrier to PrEP uptake among African American men,” with stigma throwing up another obstacle.

Photo of Raniyah Copeland and Phill Wilson by Lisa Allen
“Medical mistrust is not just something that is being made up. Black people, people of color have long history of medical abuse by American institutions and individuals,” Oakland says. “The Tuskegee Experiment is the hallmarker for many Black communities—and many Black folks don’t actually know what Tuskegee was – they can’t tell you the details of what it was.
“But what it stands for is the many experiences that we all can tell you – medical mistrust and medical abuses that have happened: forced sterilization of women, forced hysterectomies, the subpar care that many same-gender-loving people receive today, the experience that trans people have on a regular basis and medical abuses they experience. And so there is a long legacy of it and it currently happens today with improper medical care,” Copeland says.
“When we talk about the tools to end the HIV epidemic, many of those tools are based in biomedical science. But for the work we do— you have to first affirm that absolutely—that Black people, that communities of color have been abused by medical systems for eons,” she says. “You can take it all the back during slave trade. And now today that we have many more institutions to ensure that doesn’t happen again, we have to take advantage of these tools that we know are so important and can save lives. PrEP is one of those and there is absolutely a huge amount of mistrust when it comes to PrEP and Black communities.”
Copeland may helping re-frame the approach to empowering people who are living with HIV to know about sexual health but the passion to put out the fire burns just as bright as when Wilson first issued the call.
“He’s been such a huge game-changer,” Copeland says of Wilson, “and I’m very, very honored to come after him.”
AIDS and HIV
Community is the cure: AIDS Walk LA returns to fight HIV and funding cuts
AIDS Walk Los Angeles returns to West Hollywood on October 12 with the theme ‘Community Is the Cure,’ highlighting the vital role of unity, radical community action, and advocacy in the fight against HIV/AIDS, stigma, and government funding cuts

APLA Health, a nonprofit providing HIV care, prevention, and sexual health services, announced the return of AIDS Walk Los Angeles on Sunday, October 12, 2025, starting from West Hollywood Park. This year’s theme, “Community Is the Cure,” emphasizes the role of unity in advancing progress against HIV/AIDS and supporting those affected.
Walk day will feature a live performance from RuPaul’s Drag Race star Heidi N Closet, DJ sets, and community booths. Following the celebration, walkers will make their way through the streets of West Hollywood.
“This event was born out of urgency, and it’s just as relevant today,” said Craig E. Thompson, CEO of APLA Health. “We’ve made incredible progress in the fight against HIV, but that progress is under direct threat from funding cuts and political attacks. Now is the time to show that we won’t be silenced or set back.”
Since its inception forty years ago, AIDS Walk Los Angeles has grown into one of the largest HIV/AIDS fundraising events in the world, raising nearly $100 million. Proceeds fund APLA Health’s services, including HIV specialty care, sexual health services, food and nutrition support, and housing assistance.
“The HIV/AIDS epidemic has always shown us that progress happens when people come together, when patients, neighbors, families, activists, and health providers stand shoulder to shoulder. Today, with funding under attack and stigma resurfacing, unity is not optional. ‘Community Is the Cure’ is a reminder that science alone isn’t enough. We need collective willpower, advocacy, and solidarity to ensure everyone has access to the care and dignity they deserve,” Thompson said.
Cuts to Medicaid, the Ryan White Program, and prevention funding threaten access to medications, housing assistance, and food security. “Here in Los Angeles, where tens of thousands rely on these programs, even modest reductions can push people back into crisis. AIDS Walk Los Angeles helps fill some of those gaps, but philanthropy cannot fully replace the government’s responsibility,” Thompson explained.
Communities of color, the medically underserved, people living in poverty, and those experiencing homelessness are disproportionately affected. “The barriers aren’t medical. They’re structural: stigma, lack of insurance, unstable housing, and underfunded safety-net services. The administration is underinvesting in the very programs designed to break down these barriers. Until that changes, inequities in HIV prevention and care will persist,” he said.
Funds raised by the walk provide housing, groceries, case management, and access to medical care. Thompson shared the story of one patient who had lost housing and had to choose between medication and meals. “Through AIDS Walk–funded programs, we were able to connect him to stable housing, consistent medical care, and our food pantry. Today, he is virally suppressed, working again, and mentoring others who are newly diagnosed with HIV. Stories like his are common, and they remind us that cuts aren’t just numbers on a spreadsheet, they’re setbacks in real people’s lives.”
Beyond fundraising, AIDS Walk LA is a platform for advocacy. “When thousands of people flood the streets of West Hollywood, it’s a visible reminder to our community that HIV/AIDS has not gone away and to policymakers that their decisions have life-or-death consequences. The walk puts pressure on elected officials to fund programs, fight stigma, and stand up for people affected by HIV,” Thompson said.
He urged the public to take action beyond walking and donating. “Call your elected officials. Demand that HIV services remain fully funded. Show up for community hearings. Support housing initiatives. Share facts on social media to counter stigma. And, importantly, talk. Without continued conversation about HIV/AIDS and sexual health, we jeopardize the incredible advancements we’ve made in HIV care and prevention.”
Thompson also framed the walk as part of a broader activist approach. “Radical action today means showing up for one another in tangible ways, housing someone, feeding someone, advocating for someone, and refusing to accept policies that erase people’s humanity. As our theme emphasizes, when politicians fail us, COMMUNITY IS THE CURE. For participants in AIDS Walk LA, it means recognizing that the walk is just the beginning. Each person can be a messenger, an advocate, and an ally in daily life. When we work together to get people connected to support services, the collective action is radical because it insists on care and dignity in a time when those values are under attack.”
“Activism ensures policymakers cannot quietly dismantle programs. Community solidarity means that no one gets left behind. Public pressure creates accountability. When thousands unite at AIDS Walk LA, it demonstrates the broad mandate to keep fighting until HIV is no longer a public health crisis. That unity is as important as any medical breakthrough,” Thompson concluded.
For more information on AIDS Walk Los Angeles and how to register, visit https://AIDSWALK.LA.
AIDS and HIV
“If not now, when?” Journalist and activist Karl Schmid is reshaping how we talk about HIV/AIDS
The Blade sits down with the award-winning host to talk about stigma and his latest initiative – taking HIV education onto the runway

Karl Schmid has long been a staple in queer news and media. Hailing from Australia, Schmid grew accustomed to the limelight from a young age, and eventually made a successful transition into American network television through his work on red carpets for ABC.
In 2018, he would be thrust into the spotlight for a different reason. Despite repeated warnings from professional acquaintances, Schmid came out as HIV positive to share his story, wear down stigmas, and to educate people about important and misunderstood science like the concept of undetectable equals untransmittable.
And so, Schmid would grow accustomed to renewal. In 2019, he launched Plus Life Media, a platform that shares HIV resources, education, and stories of resilience from people living with HIV/AIDS. He was part of the team behind the Emmy-nominated short documentary, Marty’s Place: Where Hope Lives: an intimate look into a housing cooperative created in the 1990s to support people with HIV/AIDS. Late last week, he flew to New York for the U.S. debut of his latest initiative: HIV Unwrapped. The project pairs researchers and scientists in HIV studies with fashion design students, culminating in a runway show that features bold reimaginings and interpretations of crucial science.
The Blade spoke with Karl about the cross-pollination in his own life and career, and how his latest effort is shaping the way he blends activism and media to reinvigorate conversations around HIV/AIDS.
HIV Unwrapped feels like a really interesting pivot into a different kind of modality and platform for you. Can you tell me more about the initiative and how it fits into your legacy of activism and work?
Well, HIV Unwrapped came out of Australia and this wonderful activist named Brent Allan, who I’m good friends with. And Brent had been at, I think, the WorldPride, or something that was happening in Australia, and there was an exhibition where they paired some engineers and science people of varying professions with a fashion designer to try and illustrate their work.
And he thought, “Wow, what a great way to maybe try and interpret HIV science and reignite the conversation around HIV.” So it started in Melbourne, Australia, and it was successful there. And then they did a version in the UK earlier this year. And then in July for the International AIDS Conference that took place in Kigali, in Rwanda, they did a version.
And that’s kind of where I stepped in. I think with HIV Unwrapped, you’re drawn into the fashion first — and then the science comes. It’s just a really unique and different way of reframing the conversation about HIV. But beyond that, it’s also working with fashion students, young people, and to see them become so invested in HIV science. That’s what gets me the most excited. Because you’re opening a whole new world to a person who doesn’t maybe really think about HIV all that much, and now they’ve learned all this amazing stuff. Suddenly you’ve got a whole new bunch of people talking about HIV in exciting and fresh ways, and they’re telling their friends and they’re having conversations about it.
You’re trying to create different entry points for people to not only talk about the science behind HIV and AIDS, but also how we can reinterpret it in original and visually interesting ways.
I mean, look, you’ve got the House Appropriations Committee willing to advance this “Big Beautiful Bill” that slashes $2 billion in HIV funding in this country, and as someone living with HIV, you keep going, “Why would they do that? Why? We are so close to ending HIV.” All of a sudden, we’ve stopped funding research, and we’re stopping this, and I’m just like, “Why?”
Now more than ever, we’ve got people and politicians and government and a large part of the United States who think, “Oh yeah, HIV isn’t a thing anymore. It’s not important.” Well, it is still a thing. It is still important, and HIV Unwrapped is a way to be creative and open new avenues of dialogue.
A friend of mine sent me a handwritten note the other day. This is in Texas. One of his roommates wrote a handwritten note to another roommate, saying, “Oh, just so you know, ‘such and such’ has AIDS. So I’d be scrubbing the shower if I were you after he uses it. I personally have decided to go and shower at the gym.” And this is a person in their 30s, so we’re still having these dumb conversations from 1984.
That’s why I do what I do with Plus Life, and that’s why I’m like, “Wow, HIV Unwrapped is another tool in our toolbox we can use.” And I guess our hope is really that scientists will see this across the country and around the world and go, “Well, that is a really cool way to explain my science and make it accessible,” and want to engage in future projects like this.
How queer communities are represented in the media can leave deep imprints. I was watching an older interview you did where you recall this HIV ad you saw in a movie theater as a kid. The Grim Reaper’s there, and it’s creepy and sinister. It seems like we’ve moved away from that kind of imagery — but it doesn’t feel like we’ve necessarily come to a much better understanding of HIV/AIDS. Where do you think we’re at now in terms of representation?
The fact that, to this day, I can tell you where I was, what the movie was, that it was a Saturday, which cinema it was in, and I was a seven year old kid. It gives you an idea of how burned into my memory that is. And, I agree. I think we’ve moved away largely from the fear tactics, but we’ve stopped talking about it. I’d like to think that we’ve gotten better in representing people living with HIV, on television and film, as just people living with HIV. Where HIV doesn’t become the central storyline, and it’s not a doom and gloom, “woe is me” story. It’s just part of who they are.
But we sort of dance around anything that’s to do with our bodies or sex or sexuality, because it makes us uncomfortable. And so when I pitch stories to ABC and other networks, and even, quite frankly, trying to get press to cover HIV Unwrapped: we get passed on. People don’t want to talk to us because HIV isn’t sexy. As long as we keep doing that and having that reaction — if we don’t talk about it — we don’t get to a place where we can be comfortable with it.
Since I came out about my status all those years ago, my focus has been trying to normalize the conversation. That’s how we grow, and that’s how we learn — whether it’s HIV, whether it’s politics, whether it’s anything. But if we don’t talk about it, and we sort of pretend it doesn’t exist, and then we cut funding for it, and we sort of sweep it under the rug: it ain’t going to go anywhere.
Women of color, Black and brown women, have the highest infection rates in the United States. In the south those rates keep going up and up and up, and now we’re cutting funding to testing and to counseling and to services. I’m really worried that we will end up back with AIDS wards in hospitals again, and there’s no need for it.
To bring it back to HIV Unwrapped, that’s why, if I can come up and work with an amazing group of people to tell stories and to have conversations in fresh ways, then I’m going to keep doing it — whether it’s HIV Unwrapped, whether it’s what I do on Plus Life, whether it’s a television show or whatever crazy thing I come up with next.
It feels like there’s so much watering-down in terms of conversations around sexual health, HIV and AIDS. What is the resistance that you’ve faced, and how has that resistance changed over the years?
I’ve heard, “I think what you’re doing is great. It’s just not the right time to tell the story.” Well, when is the right time to tell the story? I think so many people in America think HIV doesn’t affect them. And the reality is very different. HIV affects everybody. If not now, when? People are still dying in this country. People are afraid to get tested, and they’re living in shame. And they’re hiding what’s wrong with them because of the stigma — and that just shouldn’t be happening.
I’ve said this a million times too. You know, HIV and AIDS doesn’t kill you. That’s not what’s going to put me in the grave. But it’s the stigma. It’s the bigoted, out-of-date opinions of Congress and politicians and public figures and uneducated people who just think this is somehow some deviant, dirty “sex disease” or drug disease, and those of us who get it deserve it. And you know, television networks, especially, are in the business of making money. And to do that, they sell advertising, and so they’re worried that advertisers will turn off if you talk about this kind of stuff.
And I think it’s maybe a little bit the opposite. I think if you can find, again, engaging and interesting ways to have real conversations, I’ve certainly found that you get a very vast and wide audience of people who will chime in and may have an opinion. And again, our opinions may differ, and that’s okay, but, but as long as we’re having the conversation, the more you say it, the less scary it is.
Almost 20 years after you were first diagnosed with HIV, do you see yourself pivoting now to work more on activism? Is that something you’re trying to focus more on now at this point of your career?
I will say that I’m incredibly fortunate to have worked for as many years as I have in broadcast, and I’ve done some really amazing things, and had some phenomenal opportunities going to the Oscars and doing all those red carpets and celebrity interviews all over the world. They’re all valuable experiences that I’ve been able to build upon. But I will say that in the last sort of two years, especially, my focus has become more about Plus Life and doing these kinds of stories and these kinds of initiatives.
I am fascinated by people. I think to be a decent journalist or broadcaster, you have to have that innate curiosity. And I am deeply curious about people and people’s behavior and where they come from, and what kind of homes they grew up in, what their friends are like. It’s incredibly satisfying to me. Do I miss being on regular, scheduled programming and television? Sure. It was a fantastic platform, and there’s nothing quite like the thrill of live television for me, and that’s why I loved being in news and entertainment news.
I think as I sort of get older, and I’m no longer the young kid on the block, and I’m not so nimble with my thumbs and my forefingers when it comes to putting stuff up on social media and Tik Tok and all of that…If I’ve got an opportunity to really hone in on the stuff that I do with Plus Life, there’s nothing more rewarding than that, right?
A behind-the-scenes documentary of the U.S. debut of HIV Unwrapped will be available to stream on November 30th, just before World AIDS Day.
AIDS and HIV
Assemblymembers urge Governor Newsom to sign “lifeline” bill for HIV medication
AB 554 amends existing law that restricts access to PrEP medication

On September 10, Assembly Bill (AB) 554, or the PrEPARE Act (Protecting Rights, Expanding Prevention, and Advancing Reimbursement for Equity Act), was passed with a majority vote by the California State Assembly and Senate. Today, the bill’s leaders are urging Governor Newsom to sign it into law.
“With a powerful coalition behind AB 554, we were able to get this bill through the process swiftly, and are hopeful that the Governor will see the need for the LGBTQ+ community,” Los Angeles Assemblymember Mark Gonzalez, one of the bill’s co-authors, told the Blade.
AB 554 was first introduced in February, and was penned by Assemblymember Gonzalez and San Francisco Assemblymember Matt Haney. It was formed to amend existing laws around health insurance coverage that currently restrict access to certain antiretroviral drugs, or HIV preventative medicine like PrEP and PEP, and to ease difficulties community clinics face in administering these medications and receiving reimbursement. The bill will also require health care plans to cover FDA-approved HIV medication without enforcing prior authorization or step therapy.
For Gonzales and the bill’s supporters, AB 554 is about boosting access to various forms of effective HIV preventative medicine and providing a safeguard for people as the state of HIV research and treatment enters unsteady ground. This all comes in the midst of the debate around the House Committee on Appropriations’s 2026 Departments of Labor, Health and Human Services, and Education, and Related Agencies funding bill, which proposes $1.7 billion in cuts to domestic HIV prevention and research efforts, as well as programs that provide care for people living with HIV/AIDS — particularly, low-income people of color.
Assemblymember Gonzalez stated to the Blade that this is a “stark reminder that this epidemic still hits our communities of color the hardest,” and wants to address this by evolving and updating laws to reflect local needs. He is hopeful about the Governor’s impending response, and stated that the bill is “not just a policy; it is a lifeline.”
“It’s about giving people real choices, equipping small clinics with the tools they need to protect lives,” Gonzalez continued, “and ensuring that California continues to put public health over politics.”
AIDS and HIV
Local organization aims to support and assist Black LGBTQ+ community
REACH LA is stepping up their mission amid hostile administration
REACH LA, a Los Angeles-based nonprofit organization aimed at working with youth of color, is stepping up their prevention resources during Black History Month to support the LGBTQ+ community of color.
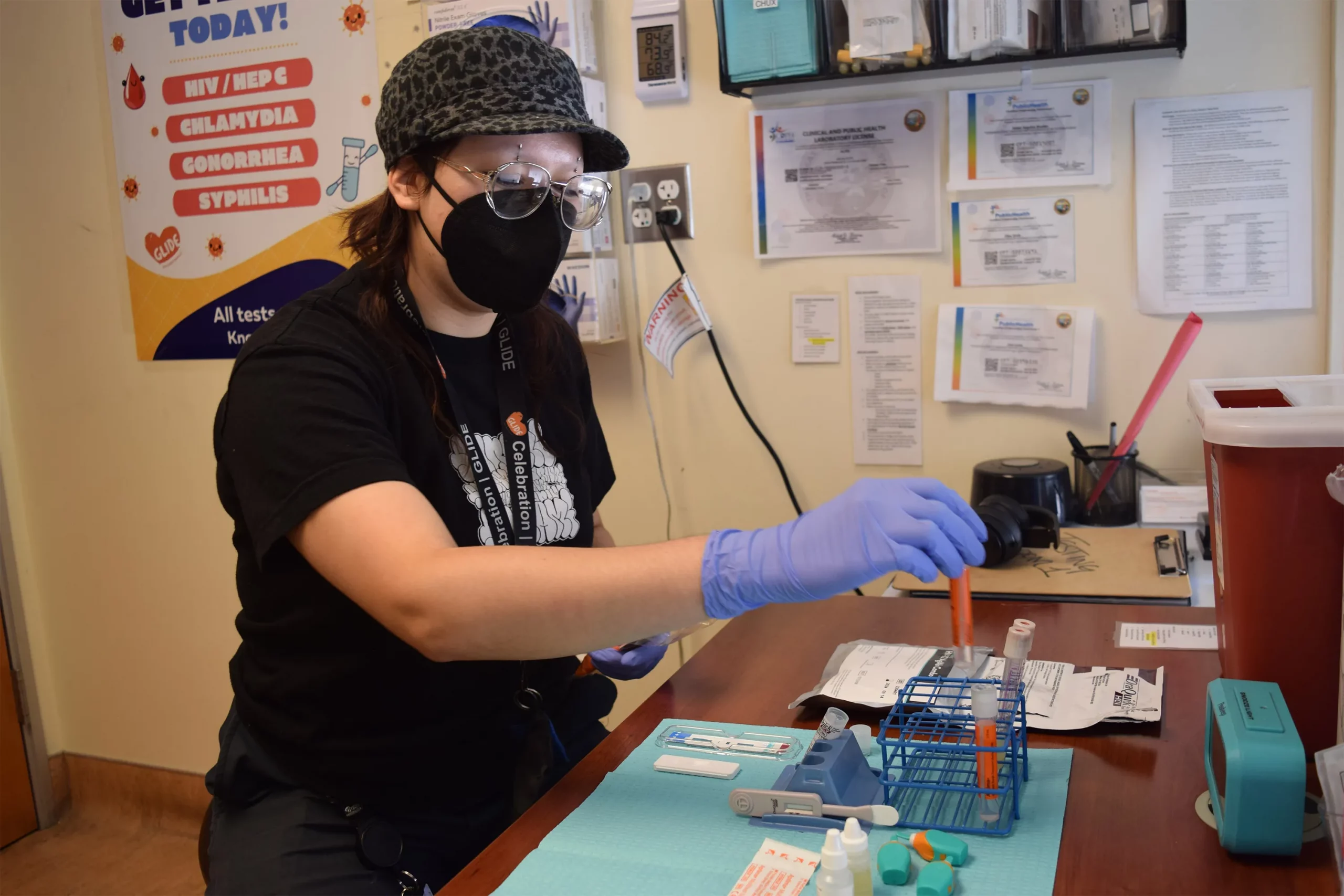
Though today is National Black HIV/AIDS Awareness Day, REACH LA works year-round to provide resources to their community members.
This month, the organization is amplifying its mission to support Black LGBTQ+ youth by offering free HIV testing and care throughout February, offering a $25 gift card as incentive to get tested. This and all of REACH LA’s efforts are geared toward assisting the marginalized Black and Latin American communities by reducing stigma, increasing education and assisting community members with resources.
The QTBIPOC community is especially vulnerable to political and personal attacks. As we head into the next four years under a hostile administration whose goal is to erase queer and trans people, there will be continued attacks on federal funding and on any other front possible.
“This year, it is especially vital, more than ever, to amplify and commemorate National Black HIV/AIDS Awareness Day. At REACH LA, we are currently engaging with individuals and partnerships while navigating through dire and uncertain times where HIV/AIDS awareness prevention efforts, access, and visibility have been under attack and restricted,” said Jeremiah Givens, chief marketing and communications officer at REACH LA.
It is important to spotlight the intersection between health equity, Black LGBTQ+ empowerment and community-based solutions during Black History Month and every other month throughout the year and especially during this particularly vulnerable time.
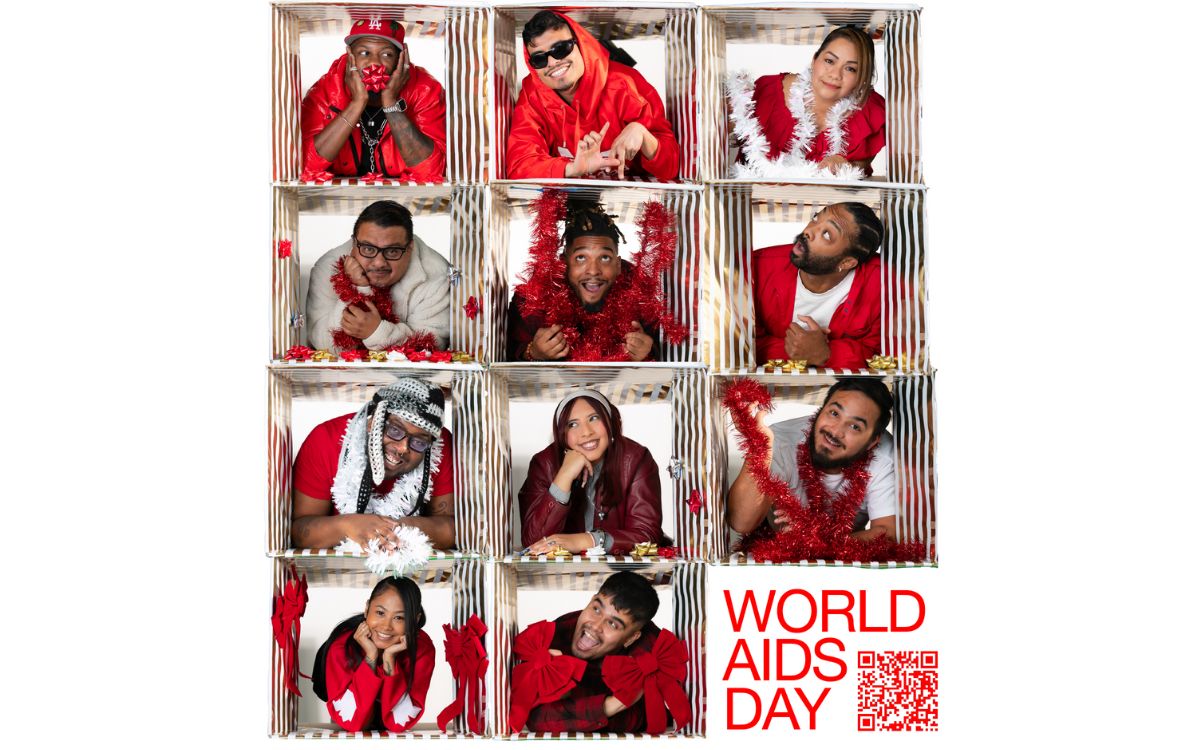
As one of eight CDC PACT Program Partners, REACH LA celebrates National Black HIV/AIDS Awareness Day with a Positive Living Campaign in collaboration with the CDC’s Let’s Stop HIV Together initiative. The campaign highlights the resilience of individuals living with HIV and works to raise awareness and foster community support.
To learn more about resources, visit their website or stop in for testing, support and other resources. The organization’s doors are open Monday through Friday, from 11 AM to 7 PM for free, on-site HIV testing and assistance with accessing PREP and PEP, linkage to care and free mental health therapy.

Over 300 people gathered last Monday to commemorate World AIDS Day in an event hosted by Bienestar Human Services. The non-profit focuses on identifying and addressing emerging health issues faced by Latinx and Lesbian, Gay, Bisexual, Trans Queer and more (LGBTQ+) populations.
The main objective of the annual event was to light a candle to honor those who passed away due to Human Immunodeficiency Virus (HIV) and celebrate those who, despite the condition, keep going.
HIV is the virus that causes Acquired Immune Deficiency Syndrome (AIDS). Once you have HIV, the virus stays in the body for life, and while there is no cure. There is, however, medicine that can help people stay healthy, states Planned Parenthood. HIV destroys the cells that protect the human body from infections. If a person doesn’t have enough of these CD4 or T cells, the body can’t fight off infections as normal. This damage can lead to AIDS, which is the most serious stage of HIV, and it leads to death over time.
In the U.S., there are about 1.3 million people newly infected with HIV in 2023 and 39.9 million living with HIV, according to the Joint United Nations Programme on HIV/AIDS.
Living with HIV for decades
Among the participants at the event at the Ukrainian Culture Center on Melrose in East Hollywood was Marcela, a transgender woman who was diagnosed HIV positive 33 years ago. She said when she learned about her diagnosis, she was so depressed she tried to commit suicide. She ended up at the hospital, and after getting better, she heard about an organization that was helping people with health issues such as hers.
“Since then, I learned to live with this condition because it is not an illness; it’s a condition,” she said.

Bienestar celebrated the World AIDS Day on December 2, 2024. (Courtesy of Bienestar)
Marcela, who didn’t provide her last name, said she not only found a new way of living with HIV but also found an extended family at Bienestar. They have guided her on how to receive the proper treatment and medicines, to be part of a support group and even to pay her rent when she needed it the most.
The 64-year-old woman doesn’t have any family members in the United States. She said five years ago, her husband passed away of pneumonia. She was living alone in Long Beach and got behind her payments during the pandemic. She said Bienestar helped her apply for a grant of over $20,000 that secured the payment for her rent, and now she is debt-free.
“I’m extremely grateful to them and all the help they provide,” she said.
Working for the community
This year, Bienestar is celebrating 35 years of serving the LGBTQ+ community. Among the many programs they offer is the Support Group for Transgender Women, which Marcela belongs to.
Mia Perez, the support group manager, said 15 to 20 members attend the group every Friday from 3 to 5 p.m. They talk about their feelings, share experiences, and plan and participate in social events.
Perez said one of the participants’ biggest concerns is accepting reality once they have been diagnosed. “However, with all these new treatments people that are HIV positive can have a normal relationship with someone who doesn’t have HIV. It’s all about getting informed,” said Perez.
Other concerns include what will happen to them once the new presidential administration takes office since they have plans to deport immigrants and many of the transgender women are immigrants.
“That’s why we are trying to get in contact with an immigration attorney or an organization so they can keep them informed of their rights,” said Perez.
Bienestar events, like World AIDS Day, help those affected create a stronger community, and they realize the recognition is not just for those who are HIV positive but also for their families and friends.
Marcela said when she is feeling down or bored at home, all she has to do is go to Bienestar and the people there always give her a warm welcome.
“They give me coffee, they offer me lunch. Being there is like being at home,” she said.
AIDS and HIV
New monument in West Hollywood will honor lives lost to AIDS
In 1985, WeHo sponsored one of the first awareness campaigns in the country, nationally and globally becoming a model city for the response to the epidemic
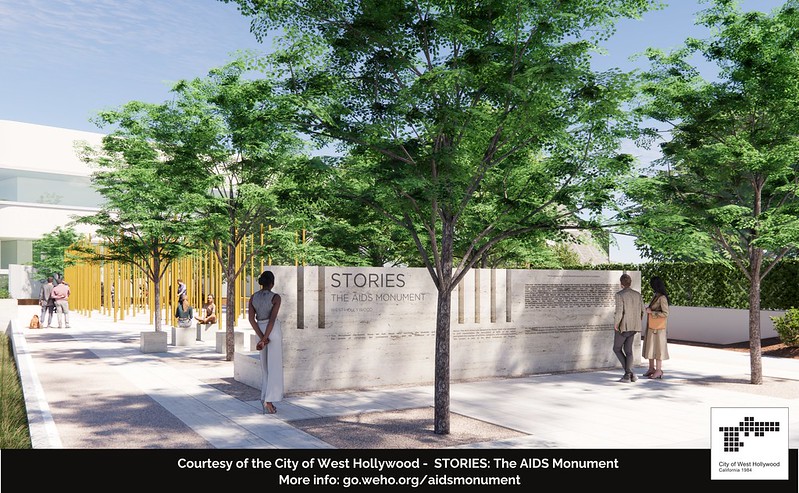
December is AIDS/HIV awareness month and this year West Hollywood is honoring the lives lost, by breaking ground on a project in West Hollywood Park that has been in the works since 2012.
Members of Hollywood’s City Council joined representatives from the Foundation of AIDS Monument to announce the commencement of the construction of STORIES: The AIDS Monument, which will memorialize 32 million lives lost. This monument, created by artist Daniel Tobin, will represent the rich history of Los Angeles where many of those afflicted with HIV/AIDS lived out their final days in support of their community.
Tobin is a co-founder and creative director of Urban Art Projects, which creates public art programs that humanize cities by embedding creativity into local communities.
The motto for the monument is posted on the website announcing the project.
“The AIDS Monument:
REMEMBERS those we lost, those who survived, the protests and vigils, the caregivers.
CELEBRATES those who step up when others step away.
EDUCATES future generations through lessons learned.”
The monument will feature a plaza with a donor wall, vertical bronze ‘traces’ with narrative text, integrated lighting resembling a candlelight vigil, and a podium facing North San Vicente Blvd.
World AIDS Day, which just passed, is on December 1st since the World Health Organization declared it an international day for global health in 1988 to honor the lives lost to HIV/AIDS.
The Foundation for the AIDS monument aims to chronicle the epidemic to be preserved for younger generations to learn the history and memorialize the voices that arose during this time.
The HIV/AIDS epidemic particularly affected people in Hollywood during the onset of the epidemic in the 1980s. The epidemic caused a devastatingly high number of deaths in the city. The city then became one of the first government entities to provide social service grants to local AIDS and HIV organizations.
In 1985, the city sponsored one of the first awareness campaigns in the country, nationally and globally becoming a model city for the response to the epidemic.
Earlier this year, the U.S. Centers for Disease Control and Prevention released the theme for World AIDS Day, ‘Collective Action: Sustain and Accelerate HIV Progress.’
The city of West Hollywood continues to strive to become a HIV Zero city with its current implementation of HIV Zero Initiative. The initiative embraces a vision to “Get to Zero” on many fronts: zero new infections, zero progression of HIV to AIDS, zero discrimination and zero stigma.
Along with the initiative and the new AIDS monument, the city also provides ongoing support and programming through events for World AIDS Day and the annual AIDS Memorial Walk in partnership with the Alliance for Housing and Healing.
For more information, please visit www.weho.org/services/human-services/hiv-aids-resources.
AIDS and HIV
National Latino AIDS Awareness Day: Breaking down stigma, silence and silos
FLAS provides HIV and STD education

When Elia Chino, Founder and Executive Director of the Fundacion Latinoamericana De Acción Social (FLAS) Inc., initially approached major HIV/AIDS agencies in Houston, Texas for support in starting an organization tailored specifically to reaching Latino populations, she was met with confusion.
“Why do you want to start a separate organization?” they asked. “We’re here!”
Chino remembers her frustration. “They didn’t understand,” she said. “Our brothers and sisters were dying, and the community needed services that they couldn’t provide.”
Indeed, in the 1990s, barriers to HIV care and treatment for Latino populations were markedly different from those faced by other populations. Information about the HIV epidemic was largely in English, and inaccessible to many individuals who had immigrated from indigenous Latin American communities and never learned to read and write in their native language, let alone English. When they were able to access treatment, Latino individuals often faced mistreatment at primary care facilities due to a lack of culturally competent care.
Perhaps most challenging was the culture of silence. Many Latino immigrants living with HIV in the United States fled homophobia, transphobia and stigma in their home countries, and were still grappling with lasting shame and guilt. Despite many people dying, there was little open discussion or education about the cause. In fact, Chino didn’t even know that the HIV epidemic took the lives of some of her best friends until speaking with their families years later.
“No one was talking about their diagnosis,” says Chino. “People had come to the United States for freedom, but still weren’t ready to talk about who they were. There was a real atmosphere of stigma, taboo, misinformation and fear.”
At the time, Chino was volunteering at a hospital serving communities without insurance. The fourth, fifth and sixth floors were all dedicated to treating people with HIV. Chino began educating herself on this crisis while she volunteered at the hospital, and founded FLAS in 1994 after discovering that the majority of HIV prevention efforts were not reaching Latino individuals.
In the beginning, without support from other organizations in the area or resources to expand, Chino was a one-woman show, conducting outreach in clubs, cantinas and bars by herself. She hadn’t anticipated the barriers she’d face as a member of the LGBTQ+ community and an immigrant. Horrible discrimination, a language barrier and intense HIV stigma in the communities she was working in made the work challenging, but also emphasized the necessity of what she was doing.
Over time, with support and funding from organizations like Gilead Sciences, FLAS has been able to expand its services from solely HIV prevention to include HIV testing, behavioral health services, housing and social services assistance, support groups and a food pantry. The organization has started hosting educational events everywhere from churches to street corners, raising awareness about HIV in the Houston community. Chino also started collaborating with the consulate of Mexico to help newcomers navigate U.S. health systems and services when they arrive in the United States. Next year, the organization will start offering mobile HIV testing clinics for communities in need.
Since its launch, FLAS has been able to expand its initial focus to address the holistic drivers of this crisis, moving beyond medical determinants of health to tackle the social and structural barriers that perpetuate the HIV epidemic and prevent Latino populations from accessing comprehensive treatment.
“Everyone keeps telling Latino individuals to get tested, but this does nothing unless you actually incentivize people to do so,” says Chino. “People have to go to work. They have to pay their rent. They have to buy food. Many can’t afford to lose their salary and spend a full day coming in to do a test or get treatment. We have to make it easier to access HIV prevention and treatment, and we have to provide incentives.”
This year marked FLAS’s 30th anniversary, which the organization celebrated with a gala in August. They have made a huge impact in Houston since their launch – providing HIV and STD education to over 500,000 Latino people, distributing over 20,000 HIV tests, referring over 40,000 people for social services and hosting over 6,000 educational events and health fairs in English and Spanish. However, many of the challenges for HIV prevention and treatment for Latino populations remain.
“We have over 30,000 individuals living with HIV in Houston, yet when we ask for people to talk about their status, no one comes forward to tell their stories. HIV is a chronic disease, but stigmatization is still so strong in the Latino community,” says Chino. “You can say you have cancer, high blood pressure, diabetes, whatever – but nobody says I have HIV. There is still so much work to do.”
As a testament to their important programming, FLAS is a recipient of funding through Gilead Sciences’ TRANScend® Community Impact Fund, a program aimed at empowering Trans-led organizations working to improve the safety, health and wellness of the Transgender community. Since its inception in 2019, TRANScend has awarded more than $9.2 million in grants to 26 community organizations across 15 U.S. states and territories.
TRANScend support has been critical to helping FLAS maintain its services. In 2020, in the midst of the COVID pandemic, Gilead’s funding helped FLAS continue to offer virtual behavioral and mental health services to the community when their physical offices had to close.
According to Chino, this type of partnership is critical to ending the HIV epidemic in Latino communities, especially for meeting communities where they are.
“Communities trust their grassroots organizations, and grassroots organizations provide for their communities,” she says. “At the end of the day, we need to continue to support the groups doing the difficult work on the ground with the people they’re serving, especially those breaking down stigma and lasting barriers to care for Latino communities.”
AIDS and HIV
40th anniversary AIDS Walk happening this weekend in West Hollywood
AIDS Project Los Angeles Health will gather in West Hollywood Park to kick off 40th anniversary celebration

APLA Health will celebrate its 40th anniversary this Sunday at West Hollywood Park, by kicking off the world’s first and oldest AIDS walk with a special appearance by Salina Estitties, live entertainment, and speeches.
APLA Health, which was formerly known as AIDS Project Los Angeles, serves the underserved LGBTQ+ communities of Los Angeles by providing them with resources.
“We are steadfast in our efforts to end the HIV epidemic in our lifetime. Through the use of tools like PrEP and PEP, the science of ‘undetectable equals intransmissible,’ and our working to ensure broad access to LGTBQ+ empowering healthcare, we can make a real step forward in the fight to end this disease,” said APLA Health’s chief executive officer, Craig E. Thompson.
For 40 years, APLA Health has spearheaded programs, facilitated healthcare check-ups and provided other essential services to nearly 20,000 members of the LGBTQ+ community annually in Los Angeles, regardless of their ability to pay.
APLA Health provides LGBTQ+ primary care, dental care, behavioral healthcare, HIV specialty care, and other support services for housing and nutritional needs.
The AIDS Walk will begin at 10AM and registrations are open for teams and solo walkers. More information can be found on the APLA Health’s website.
AIDS and HIV
Cautious Optimism in San Francisco as New Cases of HIV in Latinos Decrease
The decrease could mark the first time in five years that Latinos haven’t accounted for the largest number of new cases
SAN FRANCISCO — For years, Latinos represented the biggest share of new HIV cases in this city, but testing data suggests the tide may be turning.
The number of Latinos newly testing positive for HIV dropped 46% from 2022 to 2023, according to a preliminary report released in July by the San Francisco Department of Public Health.
The decrease could mark the first time in five years that Latinos haven’t accounted for the largest number of new cases, leading to cautious optimism that the millions of dollars the city has spent to remedy the troubling disparity is working. But outreach workers and health care providers say that work still needs to be done to prevent, and to test, for HIV, especially among new immigrants.
“I am very hopeful, but that doesn’t mean that we’re going to let up in any way on our efforts,” said Stephanie Cohen, who is the medical director of the city’s HIV and STI prevention division.
Public health experts said the city’s latest report could be encouraging, but that more data is needed to know whether San Francisco has addressed inequities in its HIV services. For instance, it’s still unclear how many Latinos were tested or if the number of Latinos exposed to the virus had also fallen — key health metrics the public health department declined to provide to KFF Health News. Testing rates are also below pre-pandemic levels, according to the city.
“If there are fewer Latinos being reached by testing efforts despite a need, that points to a serious challenge to addressing HIV,” said Lindsey Dawson, the associate director of HIV Policy and director of LGBTQ Health Policy at KFF, a health information nonprofit that includes KFF Health News.
San Francisco, like the rest of the country, suffers major disparities in diagnosis rates for Latinos and people of color. Outreach workers say that recent immigrants are more vulnerable to infectious diseases because they don’t know where to get tested or have a hard time navigating the health care system.
In 2022, Latinos represented 44% of new HIV cases in San Francisco, even though they accounted for only 15% of the population. Latinos’ share of new cases fell to 30% last year, while whites accounted for the largest share of new cases at 36%, according to the new report.
Cohen acknowledged a one-year decline is not enough to draw a trend, but she said targeted funding to community-based organizations may have helped lower HIV cases among Latinos. A final report is expected in the fall.
Most cities primarily depend on federal dollars to pay for HIV services, but San Francisco has an ambitious target to be the first U.S. city to eliminate HIV, and roughly half of its $44 million HIV/AIDS budget last year came from city coffers. By comparison, New Orleans, which has similar HIV rates, kicked in only $22,000 of its $13 million overall HIV/AIDS budget, according to that city’s health department.
As part of an effort to address HIV disparities among LGBTQ+ communities and people of color, San Francisco last year gave $2.1 million to three nonprofits — Instituto Familiar de la Raza, Mission Neighborhood Health Center, and San Francisco AIDS Foundation — to bolster outreach, testing, and treatment among Latinos, according to the city’s 2023 budget.
At Instituto Familiar de la Raza, which administers the contract, the funding has helped pay for HIV testing, prevention, treatment, outreach events, counseling, and immigration legal services, said Claudia Cabrera-Lara, director of the HIV program at Sí a la Vida. But ongoing funding isn’t guaranteed.
“We live with the anxiety of not knowing what is going to happen,” she said.
The public health department has commissioned a $150,000 project with Instituto Familiar de la Raza to determine how Latinos are contracting HIV, who is most at risk, and what health gaps remain. The results are expected in September.
“It could help us shape, pivot, and grow our programs in a way that makes them as effective as possible,” Cohen said.
The center of the HIV epidemic in the mid-1980s, San Francisco set a national model for response to the disease after building a network of HIV services for residents to get free or low-cost HIV testing, as well as treatment, regardless of health insurance or immigration status.
Although city testing data showed that new cases among Latinos declined last year, outreach workers are seeing the opposite. They say they are encountering more Latinos diagnosed with HIV while they struggle to get out information about testing and prevention — such as taking preventive medications like PrEP — especially among the young and gay immigrant communities.
San Francisco’s 2022 epidemiological data shows that 95 of the 213 people diagnosed at an advanced stage of the virus were foreign-born. And the diagnosis rate among Latino men was four times as high as the rate for white men, and 1.2 times that of Black men.
“It’s a tragedy,” said Carina Marquez, associate professor of medicine in the Division of HIV, Infectious Diseases, and Global Medicine at Zuckerberg San Francisco General Hospital, the city’s largest provider of HIV care. “We have such great tools to prevent HIV and to treat HIV, but we are seeing this big disparity.”
Because Latinos are the ethnicity least likely to receive care in San Francisco, outreach workers want the city to increase funding to continue to reduce HIV disparities.
The San Francisco AIDS Foundation, for instance, would like more bilingual sexual health outreach workers; it currently has four, to cover areas where Latinos have recently settled, said Jorge Zepeda, its director of Latine Health Services.
At Mission Neighborhood Health Center, which runs Clinica Esperanza, one of the largest providers of HIV care to Latinos and immigrants, the number of patients seeking treatment has jumped from about two a month to around 16 a month.
Among the challenges is getting patients connected to mental health and substance abuse bilingual services crucial to retaining them in HIV care, said Luis Carlos Ruiz Perez, the clinic’s HIV medical case manager. The clinic wants to advertise its testing and treatment services more but lacks the money.
“A lot of people don’t know what resources are available. Period,” said Liz Oates, a health systems navigator from Glide Foundation, who works on HIV prevention and testing. “So where do you start when nobody’s engaging you?”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
AIDS and HIV
White House urged to expand PrEP coverage for injectable form
HIV/AIDS service organizations made call on Wednesday

A coalition of 63 organizations dedicated to ending HIV called on the Biden-Harris administration on Wednesday to require insurers to cover long-acting pre-exposure prophylaxis (PrEP) without cost-sharing.
In a letter to Chiquita Brooks-LaSure, administrator of the Centers for Medicare and Medicaid Services, the groups emphasized the need for broad and equitable access to PrEP free of insurance barriers.
Long-acting PrEP is an injectable form of PrEP that’s effective over a long period of time. The FDA approved Apretude (cabotegravir extended-release injectable suspension) as the first and only long-acting injectable PrEP in late 2021. It’s intended for adults and adolescents weighing at least 77 lbs. who are at risk for HIV through sex.
The U.S. Preventive Services Task Force updated its recommendation for PrEP on Aug. 22, 2023, to include new medications such as the first long-acting PrEP drug. The coalition wants CMS to issue guidance requiring insurers to cover all forms of PrEP, including current and future FDA-approved drugs.
“Long-acting PrEP can be the answer to low PrEP uptake, particularly in communities not using PrEP today,” said Carl Schmid, executive director of the HIV+Hepatitis Policy Institute. “The Biden administration has an opportunity to ensure that people with private insurance can access PrEP now and into the future, free of any cost-sharing, with properly worded guidance to insurers.”
Currently, only 36 percent of those who could benefit from PrEP are using it. Significant disparities exist among racial and ethnic groups. Black people constitute 39 percent of new HIV diagnoses but only 14 percent of PrEP users, while Latinos represent 31 percent of new diagnoses but only 18 percent of PrEP users. In contrast, white people represent 24 percent of HIV diagnoses but 64 percent of PrEP users.
The groups also want CMS to prohibit insurers from employing prior authorization for PrEP, citing it as a significant barrier to access. Several states, including New York and California, already prohibit prior authorization for PrEP.
Modeling conducted for HIV+Hep, based on clinical trials of a once every 2-month injection, suggests that 87 percent more HIV cases would be averted compared to daily oral PrEP, with $4.25 billion in averted healthcare costs over 10 years.
Despite guidance issued to insurers in July 2021, PrEP users continue to report being charged cost-sharing for both the drug and ancillary services. A recent review of claims data found that 36 percent of PrEP users were charged for their drugs, and even 31 percent of those using generic PrEP faced cost-sharing.
The coalition’s letter follows a more detailed communication sent by HIV+Hepatitis Policy Institute to the Biden administration on July 2.
Signatories to the community letter include Advocates for Youth, AIDS United, Equality California, Fenway Health, Human Rights Campaign, and the National Coalition of STD Directors, among others.
-

 Commentary4 days ago
Commentary4 days agoFinding myself in the West Hollywood nightlife scene
-

 Los Angeles4 days ago
Los Angeles4 days agoAIDS Healthcare Foundation will celebrate its legacy of food relief at the New Year’s Rose Parade
-

 Commentary3 days ago
Commentary3 days agoLooking back on ’25. Looking forward to ’26.
-

 Features3 days ago
Features3 days agoLegendary organizing activist Dolores Huerta, 95, rides in AHF’s ‘Food for Health’ Rose Parade float
-

 Movies3 days ago
Movies3 days agoThe 25 greatest queer movies of the 21st century so far
-

 Commentary3 days ago
Commentary3 days agoNew Year, New Queer: A polite reminder of the traditions that many of us make and many of us break that are well worth revisiting this particular year
-

 Tarot Readings and Astrology2 days ago
Tarot Readings and Astrology2 days agoJanuary is calling for us to be grown-ups in Intuitive Shana’s New Year tarot reading
-

 Parks & Recreation3 days ago
Parks & Recreation3 days agoFor more than two decades, Los Angeles Neighborhood Land Trust has worked to address park inequities
-
 Books13 hours ago
Books13 hours agoA look back at the best books of 2025
-

 LGBTQ+ Youth Mental Health7 hours ago
LGBTQ+ Youth Mental Health7 hours agoLaw expanding mental health resources for LGBTQ+ youth has gone under effect






